Low-lying placenta
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
View Yuranga Weerakkody's current disclosuresAt the time the article was last revised David Martínez Juárez had no financial relationships to ineligible companies to disclose.
View David Martínez Juárez's current disclosures- Low lying placental position
- Potential placenta praevia
- Potential placenta previa
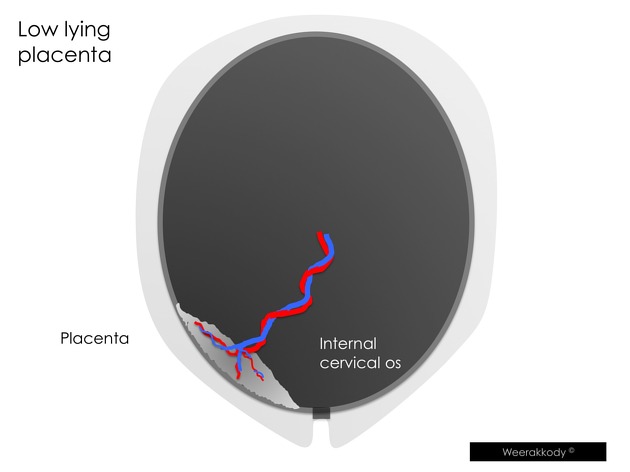
A low-lying placenta occurs when it extends into the lower uterine segment, and its edge lies close to the internal os of the cervix without covering it.
On this page:
Terminology
The term should be used when the edge of the placenta is <2 cm from the cervical internal os in pregnancies >16 weeks gestation 1,2. A placental edge >2 cm from the os is labelled normal, and a placenta covering the os is placenta praevia 1.
Epidemiology
The estimated prevalence may be as high as 10-30% of all pregnancies 3,7. The majority of placentas classified as low-lying in early pregnancy (12-14 weeks) reach a normal position on subsequent scanning later during the pregnancy due to placental trophotropism.
Risk Factors for Low-Lying Placenta
• previous caesarean section
• advanced maternal age
• multiparity
• smoking
• use of assisted reproductive technologies (ART)
Radiographic features
Ultrasound
Transvaginal ultrasound is more accurate for evaluating a low-lying placenta than transabdominal ultrasound and is safe 1,8.
Treatment and prognosis
A low-lying placenta detected on ultrasound in the second trimester typically resolves by the mid-third trimester, as such a follow-up ultrasound is recommended at 32 weeks 1. Rarely (in ~1.5% cases) it can persist to term or near term 9.
Differential diagnosis
Situations that may mimic a low lying placenta on a trans-abdominal scan includes
focal myometrial contraction(s) stretching the lower uterine segment
overdistended bladder stretching the lower uterine segment
marginal placenta praevia: especially if the placenta is posterior
Retroplacental haematoma, which may appear as a hypoechoic or heterogeneous area between the placenta and the myometrium.
vasa praevia, where fetal blood vessels run over or near the internal cervical os, potentially mistaken for placental tissue.
placenta accreta spectrum, particularly in cases where the placenta is abnormally adherent to the myometrium and extends into the lower uterine segment.
References
- 1. Reddy U, Abuhamad A, Levine D, Saade G, Saade G. Fetal Imaging: Executive Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound Fetal Imaging Workshop. J Ultrasound Med. 2014;33(5):745-57. doi:10.7863/ultra.33.5.745 - Pubmed
- 2. Jauniaux E, Alfirevic Z, Bhide A et al. Placenta Praevia and Placenta Accreta: Diagnosis and Management. BJOG. 2018;126(1):e1-e48. doi:10.1111/1471-0528.15306 - Pubmed
- 3. V. Padubidri, Ela Anand. Textbook of Obstetrics. (2006) ISBN: 9788172252236 - Google Books
- 4. Gillieson M, Winer-Muram H, Muram D. Low-Lying Placenta. Radiology. 1982;144(3):577-80. doi:10.1148/radiology.144.3.7100476 - Pubmed
- 5. Fadl S, Moshiri M, Fligner C, Katz D, Dighe M. Placental Imaging: Normal Appearance with Review of Pathologic Findings. Radiographics. 2017;37(3):979-98. doi:10.1148/rg.2017160155 - Pubmed
- 7. Chama C, Wanonyi I, Usman J. From Low-Lying Implantation to Placenta Praevia: A Longitudinal Ultrasonic Assessment. J Obstet Gynaecol. 2004;24(5):516-8. doi:10.1080/01443610410001722545 - Pubmed
- 8. Lauria M, Smith R, Treadwell M et al. The Use of Second-Trimester Transvaginal Sonography to Predict Placenta Previa. Ultrasound Obstet Gynecol. 1996;8(5):337-40. doi:10.1046/j.1469-0705.1996.08050337.x - Pubmed
- 9. Heller H, Mullen K, Gordon R, Reiss R, Benson C. Outcomes of Pregnancies with a Low-Lying Placenta Diagnosed on Second-Trimester Sonography. J Ultrasound Med. 2014;33(4):691-6. doi:10.7863/ultra.33.4.691 - Pubmed
Incoming Links
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta praevia
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynaecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumours
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumours of the testis
- testicular seminoma
-
non seminomatous germ cell tumours
- mixed germ cell tumour
- yolk sac tumour (endodermal sinus tumour)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumour
- sex cord / stromal tumours of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumour of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumours (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumours
- ureteral trauma
- other
- bladder
- kidneys




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.