Ménière disease (or idiopathic endolymphatic hydrops) is an inner ear disorder and as such can affect balance and hearing.
On this page:
Clinical presentation
One or both ears can be affected. The chief symptoms are:
episodic vertigo
sensorineural hearing loss
tinnitus
a sensation of fullness in the ears
Tullio phenomenon may be experienced 8
A 2015 joint diagnostic criteria allows for diagnoses of definite and probable Ménière disease 1:
-
definite:
two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours
audiometrically documented low- to medium-frequency sensorineural hearing loss in one ear, defining the affected ear on at least one occasion before, during or after one of the episodes of vertigo
fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear
not better accounted for by another vestibular diagnosis
-
probable:
two or more episodes of vertigo or dizziness, each lasting 20 minutes to 24 hours
fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear
not better accounted for by another vestibular diagnosis
Pathology
Although considered to be idiopathic, there is an association with inner ear effusions and endolymphatic hydrops.
Radiographic features
The role of imaging for Ménière disease is controversial 2, but a number of findings on high-resolution CT and MRI have been associated with the disease.
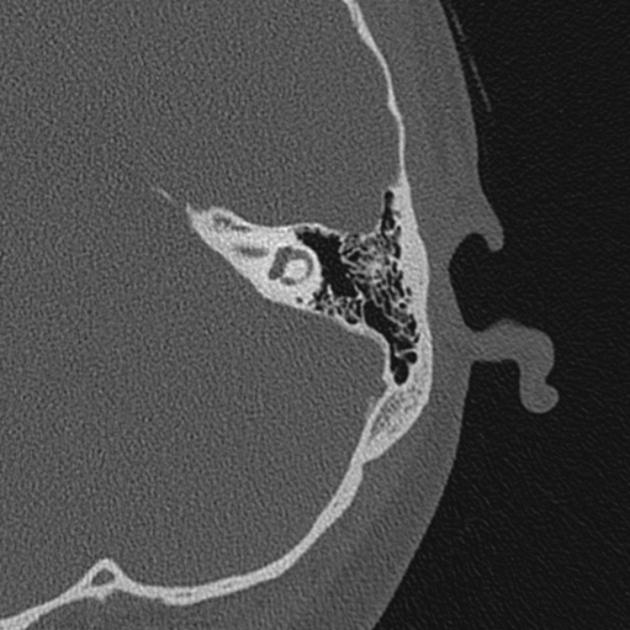
CT
At high-resolution temporal bone CT, a smaller or obliterated (non-visible) vestibular aqueduct is more often seen in ears affected with Ménière disease compared to controls 5,12,13. Moreover, a non-visible vestibular aqueduct predicts saccular hydrops on MRI while a normal (completely visible) vestibular aqueduct predicts its absence 12.
MRI
Historically, MRI has been used to exclude alternative diagnoses such as vestibular schwannoma or other cerebellopontine angle lesions, and superior semicircular canal dehiscence.
During the past decade, the morphologic substrate of Ménière disease, i.e. endolymphatic hydrops, has become visible using high resolution MRI techniques 9.
Non-contrast-enhanced MRI
Non-contrast MRI technique uses a heavily T2-weighted sequence (such as the vendor-specific sequences CISS or FIESTA-C).
The following findings have been correlated with Ménière disease or at least advanced stages of it:
elongation of the saccule (height >1.5-1.6 mm) 11,12
nonvisibility of the endolymphatic duct and sac 3
reduced fluid length within the cochlear aqueduct 14
Contrast-enhanced MRI
Contrast-enhanced techniques have emerged as a promising modality for assessment of Ménière disease. These typically use a 3D fluid-attenuated inversion recovery (FLAIR) sequence or a 3D inversion recovery (IR) sequence either 24 hours after intratympanic gadolinium administration or 4 hours after intravenous gadolinium administration 9. The latter technique is the most frequently used. The contrast material diffuses into the perilymph but not the endolymph.
The following findings on delayed post-contrast 3D FLAIR support endolymphatic hydrops, with variable performance to detect Ménière disease 9,10:
vestibular endolymphatic space (saccule and utricle) occupying >33% of the vestibule (significant if >50%)
cochlear endolymphatic space (scala media) enlargement displacing Reissner's membrane (significant if endolymphatic compartment exceeds area of the scala vestibuli)
saccule larger than utricle
History and etymology
It is named after the French physician Prosper Ménière (1799-1862) who first recognised vertigo as an inner ear disorder.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.