Paraneoplastic cerebellar degeneration is a type of paraneoplastic syndrome, and manifestation of autoimmune encephalitis, characterised by the progressive onset of cerebellar dysfunction not explained by tumoural invasion, metastasis, or treatment side effects.
On this page:
Clinical presentation
Often symptoms are present before the actual diagnosis of cancer. A significant proportion of patients (60-70%) are not diagnosed with cancer at the time their neurological symptoms first appear 4,5.
Clinical features can vary significantly. Potential symptoms include ataxia (may initially be asymmetric in 40%), dizziness, nausea and/or vomiting, diplopia, dysarthria, and/or dysphagia 1. Rapidly progressing gait unsteadiness is usually the key symptom that prompts neuroimaging. A prodromal phase featuring fever and headache can precede the main cerebellar symptoms 4,5.
Pathology
Cerebellar degeneration has been reported in patients with multiple different primary malignancies, including small cell lung cancer (most common, associated with encephalomyelitis), ovarian malignancy, breast carcinoma, and Hodgkin lymphoma 1.
There are many implicated pathogenic antibodies that may be produced by the primary malignancy to cause cerebellar degeneration, including anti-Hu, anti-Ma, anti-Yo, anti-Tr, and anti-Zic4 3.
CSF analysis
Cerebrospinal fluid (CSF) analysis typically reveals pleocytosis, elevated protein, and intrathecal IgG synthesis (i.e. oligoclonal bands). While inflammatory signs in CSF are common, they may be absent in older patients and those with specific antibodies 4,5. In seronegative paraneoplastic cerebellar degeneration, CSF abnormalities occur in 88% of cases, though oligoclonal bands appear less frequently compared to seropositive paraneoplastic cerebellar degeneration 4,5.
Some patients with paraneoplastic cerebellar degeneration have elevated 14-3-3 protein in CSF, which could be mistaken for Creutzfeldt-Jakob disease, however, in paraneoplastic cerebellar degeneration there is a characteristic double-band pattern on immunoblotting, compared to the single-band pattern seen in Creutzfeldt-Jakob disease 4,5.
Radiographic features
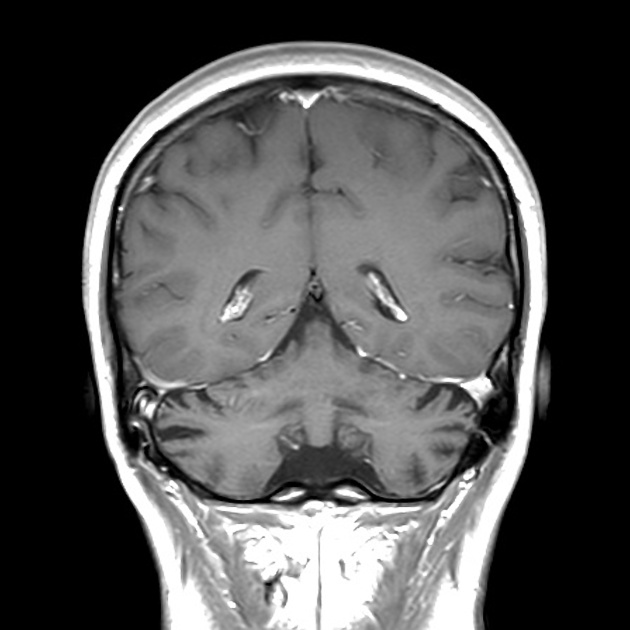
Brain imaging with CT or MRI may show either normal cerebellum, particularly in initial presentation, to eventual diffuse cerebellar atrophy. Cerebellar hemispheric enlargement and corticomeningeal enhancement have been reported 2.
Treatment and prognosis
The management is focused on treatment of the underlying malignancy, and supportive therapies.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.