Physeal arrest refers to the disturbance or complete cessation of normal growth of skeletally immature bone at the physeal growth plate due to the latter's premature closure.
On this page:
Classification
Physeal arrests can be either complete 10, i.e. premature closure of the entire physeal growth plate, or partial. Partial arrests are commonly referred to as physeal bars, or growth plate bridges wherefore the terms will be used interchangeably from here on in.
Partial physeal arrests can further be classified based on their anatomical location 4:
-
central: surrounded by a normal physis
can cause tenting and/or limb length discrepancy
if eccentric, can cause angulation
peripheral: cause angulation and can cause shortening
-
linear: surrounded by normal physis on both sides
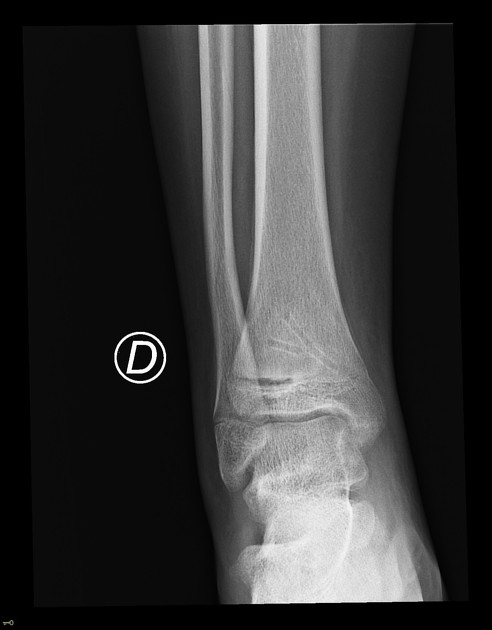
most common at the medial malleolus following Salter-Harris type III or IV fractures 5
Pathology
There are several conditions that can potentially cause physeal arrest 4,6:
-
trauma (by far most common)
-
physeal fracture; a higher number on the Salter-Harris classification is associated with a higher risk of physeal arrest
trapped periosteum in a physeal fracture 11
tibial diaphyseal fracture in adolescents 7
soft tissue physeal interposition following a fracture 9
traumatic vascular disruption
-
ischemia and osteochondroses
burns
corticosteroids
physeal bone lesion
Radiographic features
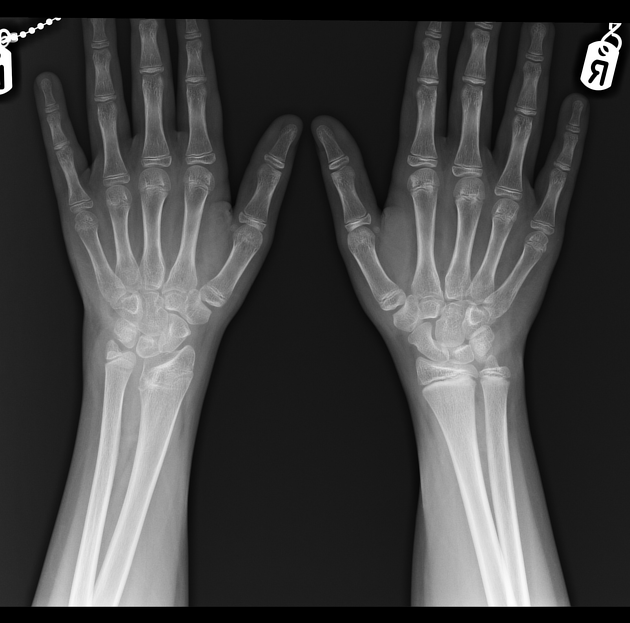
Plain radiograph
Plain film is an unreliable modality for evaluating physeal arrest. Nevertheless, an established physeal bar can be demonstrated by the presence of focal bone density bridging across the normally lucent physis.
Sequelae of physeal bars, such as bone angulation, epiphyseal displacement, and blurring of the physeal borders, may also be seen.
Sequential radiographs can be used for determining physeal arrest following a physeal fracture, especially for the assessment of limb length discrepancy: tiny metal markers are inserted into the metaphysis and epiphysis, proximal and distal to the fractured physis, and into the contralateral physis 4,10.
CT
Physeal bars can be appreciated as high attenuation bone bridges present across the normally low attenuation physis, sometimes with reactive sclerosis. Early formation of fibrous bars may be missed; additionally, physeal cartilage and surrounding soft tissue are not well visualized 9.
Sequelae of physeal bars such as bone angulation can clearly be seen.
MRI
MRI is the modality of choice, as it can detect both early (fibrous) bars and established bone bridges. A 3D spoiled gradient echo sequence with fat saturation is used to perform physeal bar mapping, wherein the physeal cartilage is bright and bone is dark 1-3,6.
Signal characteristics
-
T1
established physeal bars contain bone marrow and therefore appear as hyperintense bridges between the hyperintense epiphyseal and metaphyseal marrow ref
early fibrous bars appear as lower signal ref
T1 FS: the physeal bar appears as a focal low-intensity bridge within the hyperintense growth plate ref
T2/T2*: the physeal bar appears as a focal low-intensity area within the normal high signal physeal cartilage ref
Treatment and prognosis
Accurate mapping and sizing of a physeal bar is important for directing management 1,2,8,9. The aim of treatment is to avoid deformity and limb length discrepancy.
Management is based on factors such as anatomic location, anticipated growth as related to the patient's age, and the shape of the deformity 9.
Small bars (<30% of the physis) are managed conservatively. Medium-sized bars (30-50%) require excision of the bar. Larger bars (>50%) are usually managed with more extensive surgery 4.
A physeal bar as a consequence of a physeal tumor cannot be surgically resected; other treatment options should be sought 4.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.