Pneumoretroperitoneum is by definition presence of gas within the retroperitoneal space.
On this page:
Pathology
Pneumoretroperitoneum is always abnormal and has a relatively small differential:
-
perforated retroperitoneal hollow viscus
-
blunt or penetrating abdominal trauma 12
endoscopy +/- biopsy (rare) 3
ERCP: especially when a sphincterotomy is performed; incidence 0.5-2% 3,12
-
endoscopy +/- biopsy
-
surgery, e.g. transanal excision of rectal carcinoma 2
foreign body insertion
endoscopy
trauma
rarely an intraperitoneal hollow viscus can perforate into the intramesenteric space and then track air to the retroperitoneal spaces
-
-
residual air from retroperitoneal surgery
urological/adrenal 4
spinal (anterolateral approach) 5
If localised, and especially in the presence of an air-fluid level, a retroperitoneal abscess should be suspected.
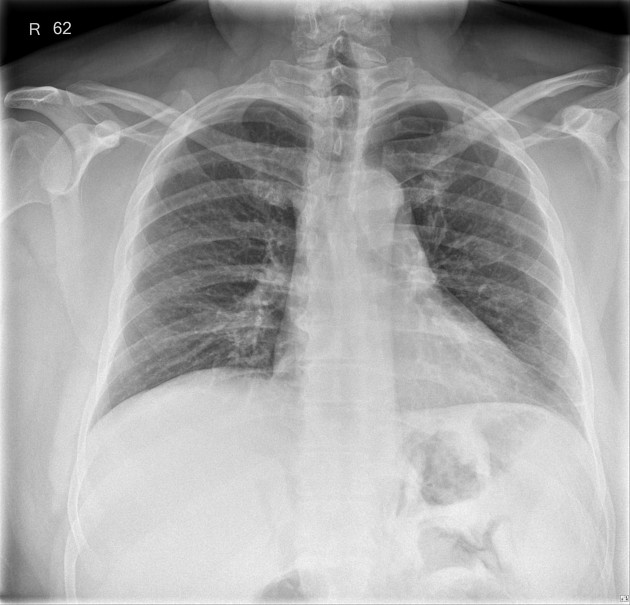
Radiographic features
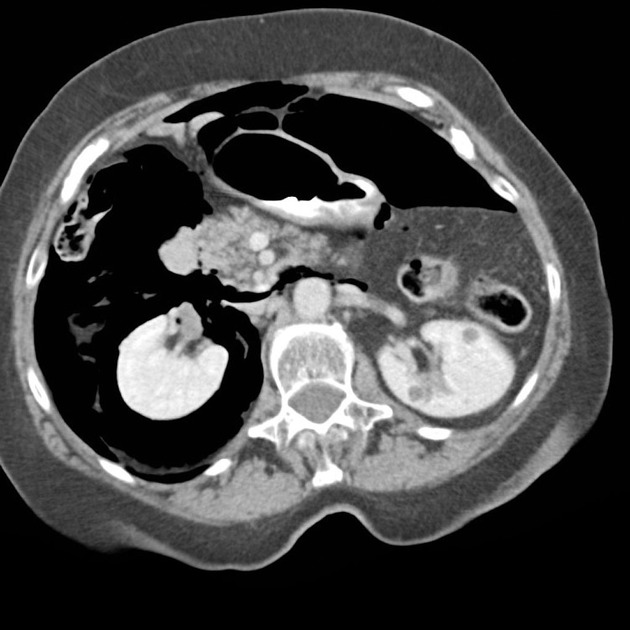
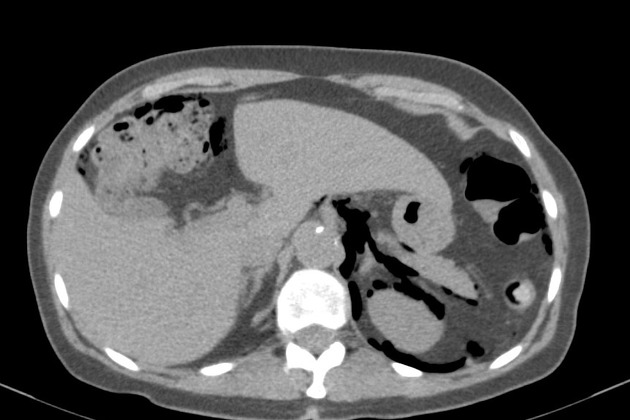
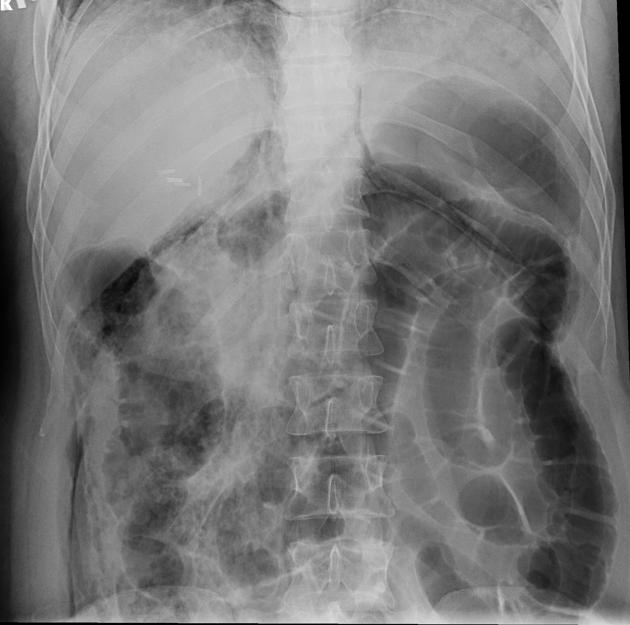
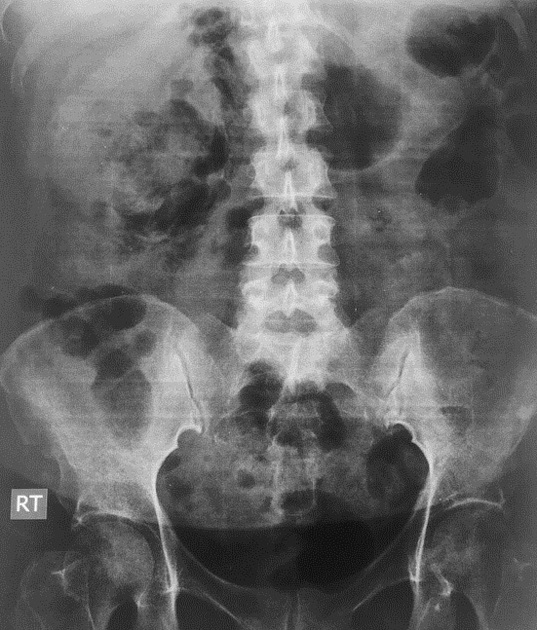
Pneumoretroperitoneum is best appreciated by CT, however, can also be detected by plain abdominal radiograph and even by transabdominal ultrasound. Generally, the air is most commonly seen surrounding the kidneys in the right and left upper quadrants of the abdomen 6. There may also be a loss of the normal psoas muscle shadow 6.
Ultrasound
Interfaces between free air and soft tissues appear as echogenic lines with posterior reverberation artifacts and the obscuration of far-field structures. In pneumoretroperitoneum air will collect around the following structures 10:
-
right kidney
-
referred to as the veiled right kidney sign 7
will not change appearance with patient re-positioning, as opposed to the free air in pneumoperitoneum 11
-
-
great vessels
the disappearance of the retroperitoneal inferior vena cava and abdominal aorta 9
head of the pancreas
-
gallbladder
retroperitoneal air will collect posteriorly
duodenum
Differential diagnosis
On plain radiography, the differential is that of gas in other spaces which also projects over the abdomen. It thus includes:
CT has little difficulty in distinguishing these.













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.