Polyhydramnios refers to a situation where the amniotic fluid volume is more than expected for gestational age.
It is generally defined as:
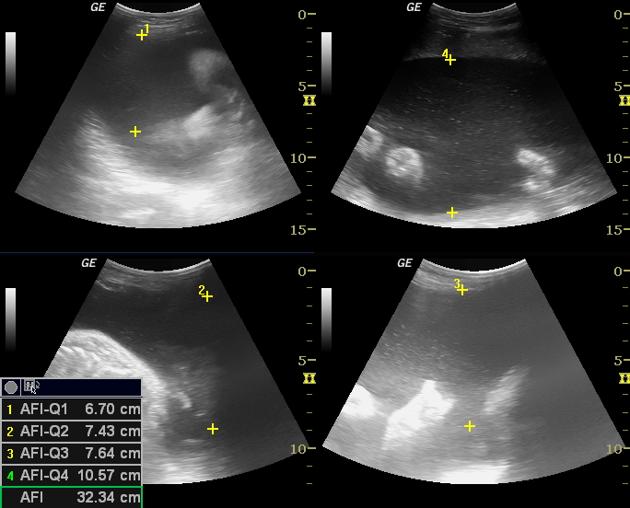
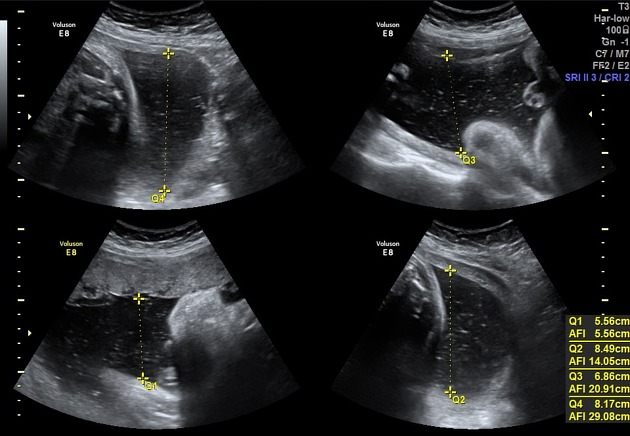
amniotic fluid index (AFI) >25 cm, though the cutoff in some centres is being reduced to 24 cm 14
-
largest fluid pocket depth (maximal vertical pocket) >8 cm 6
some centres, particularly in Australia, New Zealand, and the United Kingdom, use a cut off of >10 cm ref
overall amniotic fluid volume >1500-2000 mL 3
two diameter pocket (TDP) >50 cm 2
On this page:
Epidemiology
Polyhydramnios can occur in 1-1.5% of pregnancies ref.
Associations
fetal macrosomia: independent of maternal diabetes 2, in the idiopathic form
maternal overhydration ref
Polyhydramnios is associated with poor outcomes if present in combination with intrauterine growth restriction (IUGR); usually seen in aneuploidies 18,13, and 21 ref.
Clinical presentation
The patient may clinically present as a large for dates uterus.
Pathology
Polyhydramnios occurs as a result of either increased production or decreased removal of amniotic fluid. The aetiology of polyhydramnios can be due to a vast variety of maternal and fetal disorders.
It is usually detected after 20 weeks (often 3rd trimester).
Aetiology
The potential causes of polyhydramnios are variable including:
-
idiopathic: 60-65%
this is a diagnosis of exclusion despite accounting for a majority of cases, also termed idiopathic polyhydramnios
-
maternal: 25-30%
diabetes: commonly gestational diabetes
-
fetal: 10-20%
CNS lesions (e.g. neural tube defects): fetal CNS abnormalities tend to be the commonest out of all fetal causative associations 3
-
proximal gastrointestinal obstruction
-
gastrointestinal atresia(s)
fetal intestinal volvulus, e.g. from an intestinal malrotation
-
-
fetal cervicothoracic abnormalities
-
fetal cervical masses
-
thoracic masses
-
-
fetal cardiovascular anomalies
sustained fetal tachycardia (e.g. supraventricular tachycardia (SVT), atrial flutter, ventricular tachycardia) 12
-
twin pregnancy-related complications
twin-twin transfusion: occurs in the recipient
hydrops fetalis: immune and non-immune
-
fetal skeletal abnormalities
reduced fetal movement
Classification
This classification is general consensus based on common practices at the time of writing (July 2016) but this varies according to countries and gynaecologist association guidelines.
Some classify the severity of polyhydramnios as
mild: a single deepest pocket at 8-11 cm or amniotic fluid index (AFI) 25-30
moderate: a single deepest pocket at 12-15 cm or AFI 30.1-35
severe: single deepest pocket >16 cm or AFI >35
Treatment and prognosis
The prognosis is variable dependent on associated conditions. Usually minimal or no intervention is required for idiopathic mild uncomplicated cases. Options include:
improved maternal diabetes control
caesarian section if there is profound macrosomia
therapeutic amniocentesis/amnioreduction
indometacin 9,10
Complications
The risk of the following obstetric complications is increased when polyhydramnios is present due to over-expansion of the uterus 13:
maternal dyspnoea
premature membrane rupture
postpartum haemorrhage: due to reduced uterine myometrial tone







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.