Polymyositis is a rare autoimmune, at times considered paraneoplastic, inflammatory connective tissue disease characterised by proximal muscle weakness (myositis). It has historically been considered a form of idiopathic inflammatory myopathy. The condition is closely related to dermatomyositis, and the term “polymyositis” is often applied clinically when the condition spares the skin.
It principally affects the skeletal system but can also affect other organ systems, such as the lungs (see polymyositis - lung involvement).
On this page:
Terminology
Polymyositis is an increasingly rare diagnosis. With advances in medical science, many patients previously diagnosed with polymyositis are being reclassified as having other inflammatory myopathies, such as immune-mediated necrotising myopathy, inclusion body myositis, or anti-synthetase syndrome 5. There is conjecture among experts in the literature as to whether polymyositis still exists as a clinical entity, but if it does, it is likely very rare 5.
Epidemiology
There are several forms of the disease. The most common form affects those in their fourth decade. There is a recognised female predilection (F:M = ~2:1).
Clinical presentation
Polymyositis usually presents insidiously over a few months with symmetrical painless muscular weakness with no cutaneous manifestations (cf. dermatomyositis). Myalgia has been reported in less than one-third of the patients.
Radiographic features
Muscle involvement is usually symmetric, but not necessarily evenly distributed.
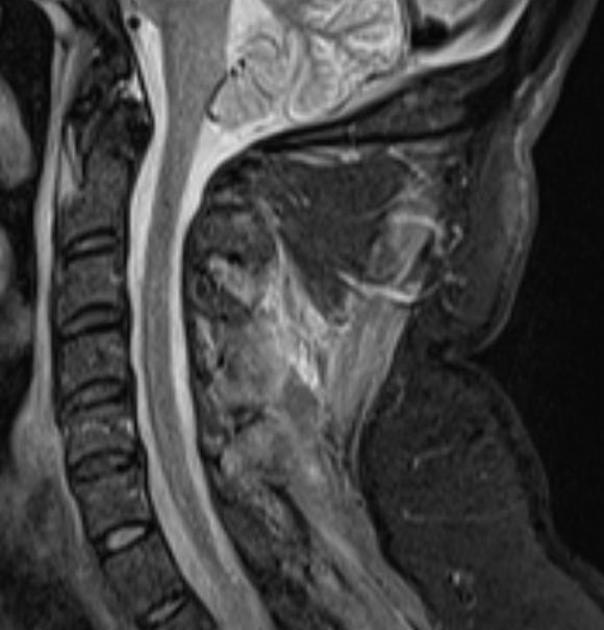
MRI
MRI has been used for diagnosis, follow-up, and to identify the best site for muscle biopsy.
T2/STIR: affected regions during active disease have high signal intensity, reflecting muscle oedema
Other features, in the chronic phase, may include 3:
fatty infiltration of muscles
muscle calcification
Treatment and prognosis
Management is with immunosuppression, similar to dermatomyositis.
Differential diagnosis
On MRI there is a broad differential:
Some differentials to consider include:
-
usually involving patients over 50 years
-
will have skin features
-
will have skin features
-
usually, will not involve all the muscular compartments and will not present with a relatively symmetrical bilateral pattern
-
collagen vascular diseases (e.g. systemic lupus erythematosus, Sjögren syndrome, and rheumatoid arthritis)
has a more focal, sometimes nodular, myositis
-
drug-induced myositis (e.g. statins, antiretroviral drugs (e.g. d-drugs) used in HIV treatment, checkpoint inhibitors)
reversible after discontinuation of the medication
-
muscular dystrophy (e.g. Duchenne)
muscles evolve from an oedematous phase to become atrophic
there is no associated skin and subcutaneous oedema





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.