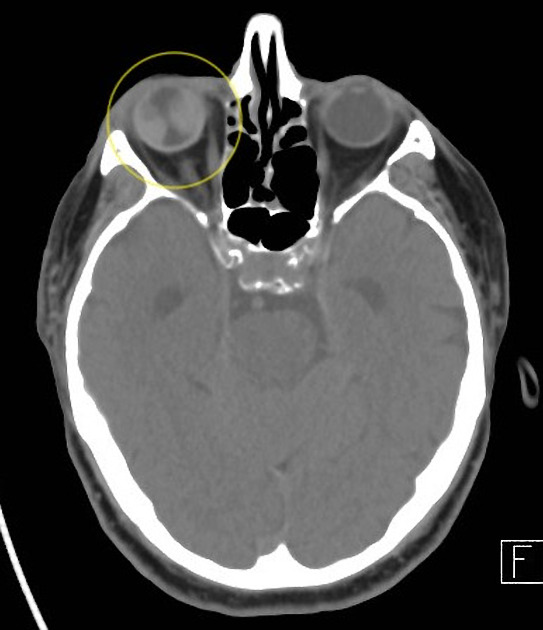
Posterior vitreous detachment (PVD), also known as hyaloid detachment, occurs when the retinal layer and vitreous body/posterior hyaloid membrane dissociate, with an intervening fluid collection forming in the subhyaloid space.
On this page:
Epidemiology
It is thought to be a common consequence of ageing, occurring in more than 70% of the population over the age of 60 years 1.
Clinical presentation
PVD is the most common cause of sudden onset "floaters" in one's visual field, most correctly referred to as "vitreous condensations" in this context. It also may cause photopsia, exacerbated by eye movements.
Radiographic features
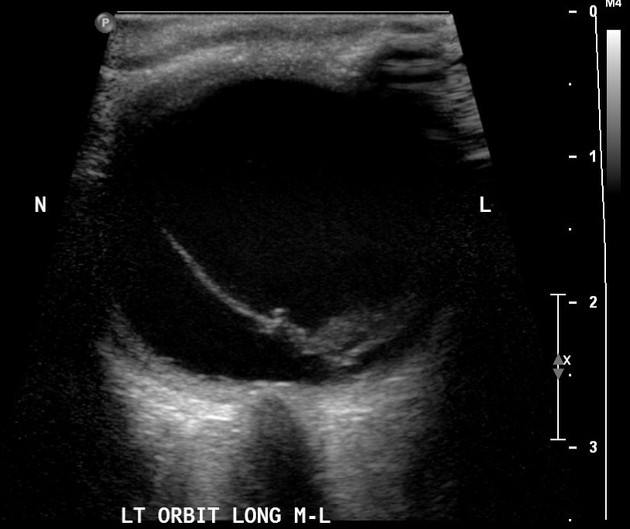
Ultrasound
The sonographic appearance of isolated posterior vitreous detachment includes the following characteristics 3:
-
linear, echogenic membrane in the posterior compartment
thickening may be observed in the presence of haemorrhage or inflammation
-
may demonstrate tethering near the ora serrata
point of attachment referred to as the vitreous base
-
freely mobile with oculokinetic ultrasonography 2
unlike retinal and choroidal detachment, the membrane will cross the intersection of the optic nerve sheath and posterior wall of the globe
in the acute stages, PVD should demonstrate prominent "after movements" that are more prominent than what would be expected from retinal/choroidal detachments 4
mobility may be lost over time, making the differentiation from other vitreous pathologies difficult
-
may be associated with other pathologic findings, including;
retinal detachment
vitreous haemorrhage







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.