Pulmonary nocardiosis is an infrequent but severe opportunistic infection typified by necrotic or cavitary consolidation in an immunocompromised patient. It is caused by Nocardia spp.
On this page:
Epidemiology
The condition is rare in healthy individuals. Immunocompromised patients with impaired cell-mediated immunity related to AIDS and transplantation are susceptible.
Increased incidence may be attributed to improved laboratory detection techniques and increasing prevalence of impaired cellular immunity 2.
Risk factors
Apart from impaired cell-mediated immunity, respiratory disorders such as chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis, previous tuberculosis and cystic fibrosis increase the risk of infection 11.
Pathology
Pulmonary nocardiosis is most commonly caused by Nocardia asteroides, which is an aerobic gram-positive weakly acid-fast bacterium distributed worldwide in soils. Other less common species include Nocardia farcinica and Nocardia otitidiscaviarum 3. It is usually acquired by direct inhalation of contaminated soil.
Location
There may be an increased upper zonal predilection 1.
Radiographic features
Due to a high rate of haematogenous spread, suspected cases of pulmonary nocardiosis should have a brain MRI to exclude cerebral abscess formation. Other organs such as liver, adrenal, skin, and soft tissues can also be involved.
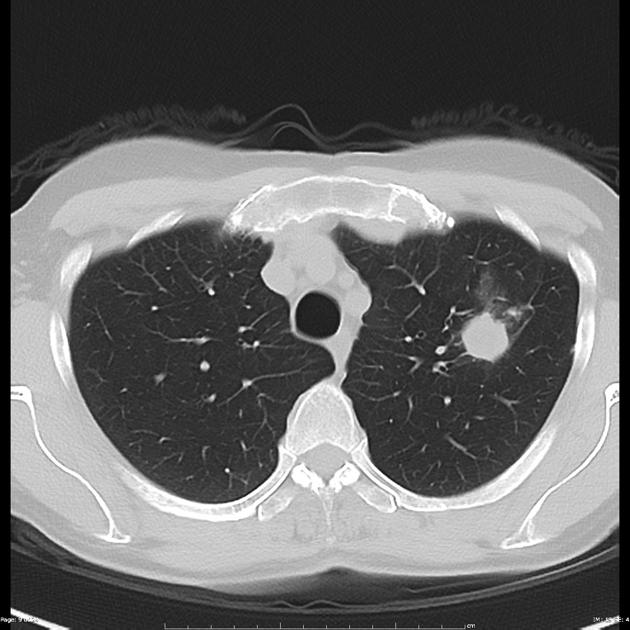
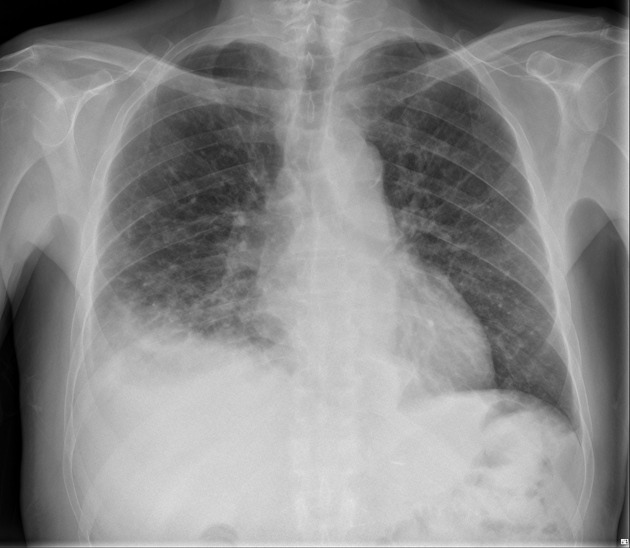
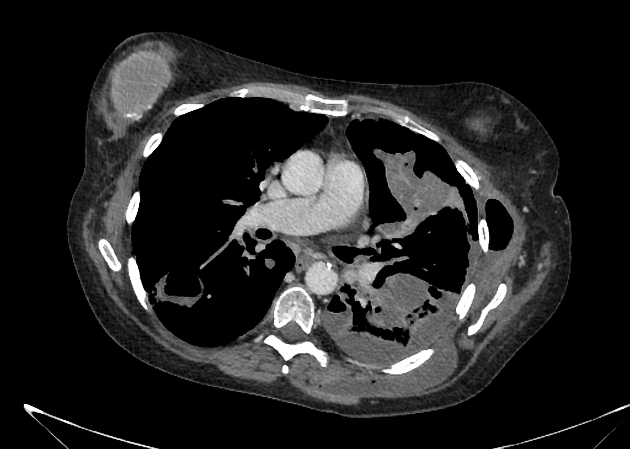
Plain radiograph / CT
There are several reported radiographic patterns which include:
-
lobar or multilobar consolidation
probably the predominant feature 4
focal areas of decreased attenuation may reflect abscess formation
cavitation in 30%
solitary lung masses and/or nodules
Other accompanying features which are non-specific on their own include:
lung cavitating lesions: may occur in up to 1/3 of patients 4
empyema necessitans: can lead to chest wall invasion 4,5
lymphadenopathy is unusual
Those with immunodeficiency may show more cavitating lesions and multiple nodules 6.
The temporal progression of radiographic abnormalities tends to be slow.
Different spread patterns have given varying features:
-
endobronchial spread
can occur with cavitation
characterised by the presence of small centrilobular nodules, often associated with bronchial wall thickening and endobronchial debris
-
disseminated pulmonary nocardiosis
numerous nodules of various sizes
Treatment and prognosis
The usual treatment of choice is trimethoprim/sulfamethoxazole (cotrimoxazole). With certain complications, surgical drainage may be required. The prognosis can vary, with those with disseminated nocardiosis having mortality rates up to 40%. Subtherapeutic levels of antibiotics can result in flare-ups while patients are on treatment.
Differential diagnosis
On imaging it can sometimes mimic:
lung cancer: in particular squamous cell carcinoma with cavitation
non-nocardial lung abscess





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.