Purulent pericarditis or pericardial empyema is a serious form of a bacterial, fungal or parasitic infection of the pericardium associated with a neutrophilic pericardial effusion.
On this page:
Epidemiology
Purulent pericarditis is rare nowadays and makes up <1% of pericarditis cases.
Risk factors
Factors that increase the likelihood of developing purulent pericarditis include 1-4:
cardiac or thoracic surgery
malignancy
preexisting pericardial effusion
Associations
Clinical conditions with which purulent pericarditis has been associated include 1-3:
Clinical presentation
Patients with purulent pericarditis are usually seriously ill and present with fever, fatigue and chest pain. On auscultation, there might be a pericardial friction rub 1-4. An electrocardiogram might show abnormalities as PR segment depression and ST elevation in all leads 2-5.
Complications
Complications of purulent pericarditis include the following 1-4:
persistent chronic pericarditis
cardiac arrest and death
Pathology
Purulent pericarditis is characterised by pus in the pericardial fluid which might show up frankly in pericardiocentesis, required for securing the diagnosis 1.
The following parameters are in favour of purulent pericarditis vs tuberculous or neoplastic pericarditis 1:
elevated pericardial white cell count (mean ≥2.8/µL)
a high percentage of neutrophils (≥92%)
elevated pericardial vs serum glucose ratio (≈0.3)
The most common organisms in western countries are staphylococci, streptococci, and pneumococci. After thoracic surgery or in immunocompromised patients, Staphylococcus aureus, fungi and anaerobes from the oropharynx are common pathogens 1.
Radiographic features
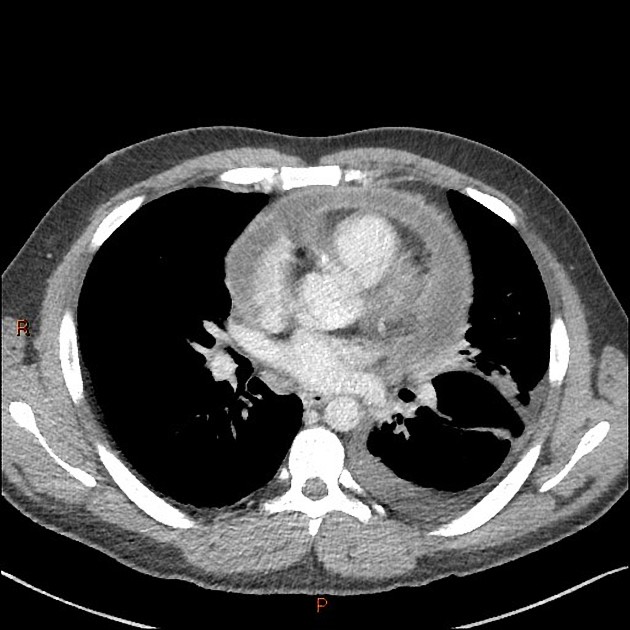
On most imaging modalities purulent pericarditis manifests as pericardial effusion 2.
Plain radiograph
Chest x-ray might show an abnormal cardiac silhouette and pleural effusions 3.
Ultrasound
Echocardiography
Echocardiography is the first-line imaging modality in the diagnosis and monitoring of therapy in the setting of acute pericarditis. It can identify pericardial effusions as well as complications as cardiac tamponade or pericardial constriction 3-5.
CT
CT will demonstrate pericardial effusion, pericardial thickening and enhancement. Additionally, it might demonstrate loculated collections and potential sources as pleural empyema or pneumonia.
MRI
MRI is an adjunctive imaging modality for pericarditis and is done if echocardiographic findings are ambiguous or if myocardial involvement is suspected. MR imaging findings include the following 5:
heterogeneous pericardial effusion
Radiological report
The radiological report should contain a description of the following:
pericardial effusion, pericardial thickening, pericardial enhancement
myocardial involvement or signs of myocarditis
Treatment and prognosis
Purulent pericarditis is a serious and dangerous condition and requires fast and aggressive treatment. Even then, the mortality rate is approximately 15%. Management includes immediate empiric antibiotic therapy until the causative microbiological agent is available on one hand and pericardial drainage on the other hand. Intrapericardial thrombolysis is an option for loculated fluids. More invasive surgical options include subxiphoid pericardiotomy with rinsing of the pericardial cavity, pericardial windowing or pericardectomy 1-3.
History and etymology
Pericardiocentesis had been already advocated by Riolanus almost 400 years ago 6.
Differential diagnosis
Conditions mimicking the radiological appearance of purulent pericarditis include 1:





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.