Rheumatoid arthritis (RA) is a chronic autoimmune multisystemic inflammatory disease that affects many organs but predominantly attacks the synovial tissues and joints.
The paediatric condition, juvenile rheumatoid arthritis, is discussed separately.
On this page:
Epidemiology
The overall prevalence is 0.5-1% and the disease is 2-3 times more common in women 1. Onset is generally in adulthood, peaking in the 4th and 5th decades ref.
Risk factors
Clinical presentation
The clinical features can be broadly categorised as articular and extra-articular. Generally, the onset of the condition may be insidious or abrupt, and early features commonly include tiredness, malaise, and generalised aches ref. Articular features generally develop prior to extra-articular features ref.
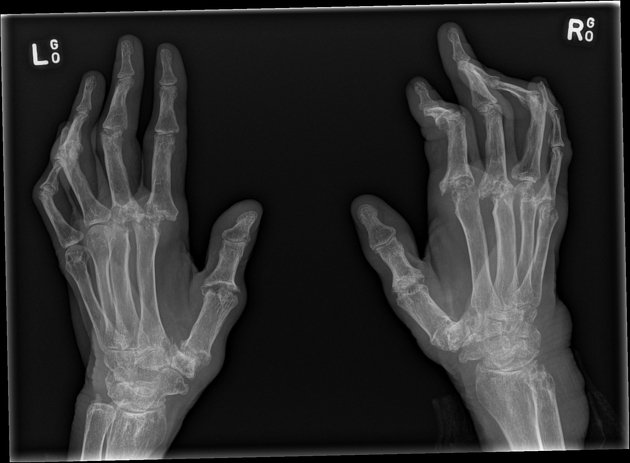
Articular features include a symmetrical deforming peripheral polyarthropathy that classically affects the fingers and hands, but also commonly involves the feet and can involve multiple other joints. The arthropathy has a classic inflammatory phenotype, with joint stiffness, reduced range of motion, reduce functionality, and a 'boggy' feel to palpation. For further details, please refer to musculoskeletal manifestations of rheumatoid arthritis.
Extra-articular features include ref:
-
interstitial lung disease
pulmonary nodules
pleural effusion
Caplan syndrome 7: rheumatoid arthritis and pneumoconiosis
-
cardiovascular involvement
accelerated/premature coronary artery atherosclerosis 8, contributing significantly to the excess mortality of RA
-
cutaneous involvement
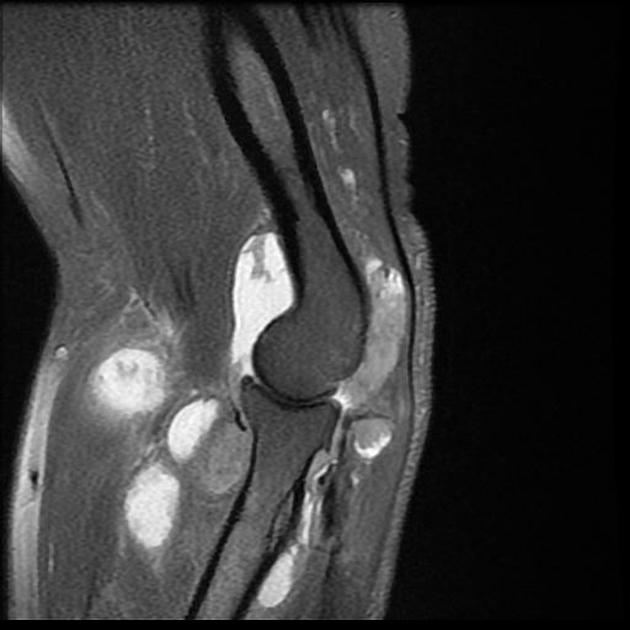
rheumatoid nodules: usually seen in pressure areas (e.g. elbows, occiput, lumbosacral) 3 in RF-positive patients 9
rheumatoid vasculitis: classically deep cutaneous ulcers in the lower limbs, may have associated nailfold lesions
-
haematological involvement
anaemia of chronic disease
Felty syndrome: syndrome characterised by the triad of rheumatoid arthritis, splenomegaly, and neutropenia
-
ocular involvement
-
neurological involvement
Pathology
Aetiology is unknown but is probably multifactorial. It is generally considered that a genetic predisposition (e.g. HLA-DR B1 which is the most common allele of HLA-DR4 involved in rheumatoid arthritis) and an environmental trigger (e.g. Epstein-Barr virus postulated as a possible antigen, but not proven) lead to an autoimmune response that is directed against synovial structures and other organs ref.
Activation and accumulation of CD4 T cells in the synovium start a cascade of inflammatory responses which result in ref:
activation of the macrophages and synovial cells and production of cytokines such as IL4 and TNF, which in turn cause proliferation of the synovial cells and increase the production of destructive enzymes such as elastase and collagenase by macrophages
activating B cell lymphocytes to produce various antibodies including rheumatoid factor (RF-IgM antibodies against Fc portion of the IgG) which makes immune complexes that deposit in different tissues and contribute to further injury
directly activate endothelial cells via increased production of VCAM1, which increases the adhesion and accumulation of inflammatory cells
producing RANKL which in turn activate osteoclasts causing subchondral bone destruction
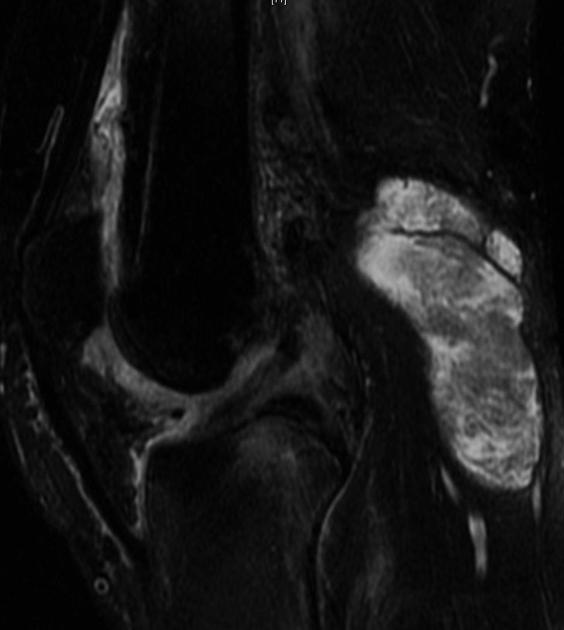
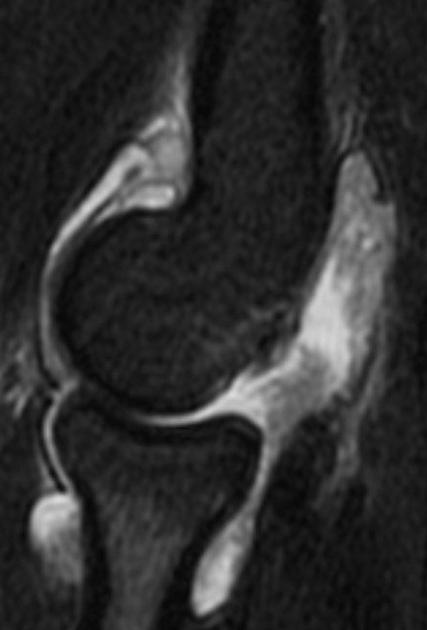
The inflammatory response leads to pannus formation. Pannus is an oedematous thickened hyperplastic synovium infiltrated by lymphocytes T and B, plasmocytes, macrophages, and osteoclasts. Pannus will gradually erode bare areas initially, followed by the articular cartilage. It causes fibrous ankylosis which eventually ossifies 2,3.
Other associated antigen subtypes include 14
HLA-B54
HLA-DQB1*0601
HLA-B40
Diagnostic criteria
Diagnosis is based on a combination of clinical, radiographic, and serological criteria. The 2010 ACR - EULAR classification criteria for Rheumatoid Arthritis 4 has a maximal score of 10 and requires a score of >6 for a diagnosis of rheumatoid arthritis to be made:
-
joint involvement
0: 1 large joint
1: 2-10 large joints
2: 1-3 small joints (with or without the involvement of large joints)
3: 4-10 small joints (with or without the involvement of large joints)
5: >10 joints (at least 1 small joint)
-
serology
0: negative RF and negative anti-CCP
2: low-positive RF or low-positive anti-CCP
3: high-positive RF or high-positive anti-CCP
-
duration of symptoms
0: <6 weeks
1: >6 weeks
Markers
There are several serological markers for rheumatoid arthritis ref:
rheumatoid factor (RF): is an IgM antibody against FC portion of the IgG antibodies, and is a traditional marker but is non-specific; associated with several autoimmune and chronic infectious diseases
anti-cyclic citrullinated peptide (anti-CCP)/anti-citrullinated plasma antibody (ACPA): it is more than 80% sensitive and more than 95% specific
elevated CRP and/or ESR
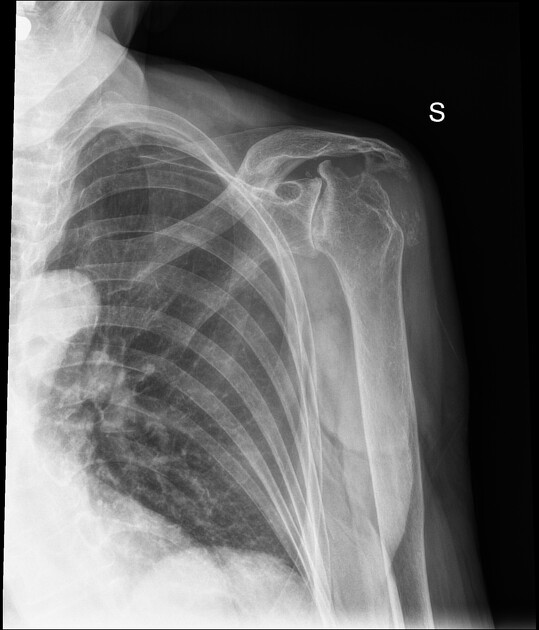
Radiographic features
Musculoskeletal
Musculoskeletal manifestations are the earliest and dominant features of rheumatoid arthritis ref.
For further details, please refer to musculoskeletal manifestations of rheumatoid arthritis.
Respiratory
Pulmonary rheumatoid disease may involve the airway, interstitium, and/or pleura; a full description is available in respiratory manifestations of rheumatoid arthritis ref.
Abdominal
Splenomegaly may be seen as part of Felty syndrome, usually in long-standing rheumatoid arthritis ref.
Treatment and prognosis
Treatment of rheumatoid arthritis is aimed at improving the symptoms and slowing disease progression. Medications used in treatment include:
-
disease-modifying anti-rheumatic drugs (DMARDs)
conventional synthetic DMARDs (csDMARDs): e.g. methotrexate, leflunomide, prednisolone
biological DMARDs (bDMARDs): e.g. TNF-α inhibitors (e.g. infliximab), tocilizumab, abatacept, rituxumab
targeted synthetic DMARDs (tsDMARDs): e.g. tofacitinib
The disease carries a significant burden of disability. There is also a reduction in life expectancy, with excess mortality usually related to its non-articular manifestations 5,6.
History and etymology
Rheumatoid arthritis was a term first coined by British physician Sir Alfred Baring Garrod (1819-1907) in 1859 11.
Differential diagnosis
psoriatic arthritis: distal distribution, new bone formation, enthesitis ref
erosive osteoarthritis: distal distribution, central erosions, and 'gull wing' appearance ref
systemic lupus erythematosus: non-erosive metacarpophalangeal joint subluxation ref
-
scleroderma 13
can have similar erosions and be CCP-positive
soft tissue calcifications and acro-osteolysis are characteristic findings





















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.