Shading sign (endometrioma)
Updates to Article Attributes
Shading sign is an MRI finding typically seen in an endometrioma. It may also be seen with some endometrioid tumours (e.g. endometrioid carcinoma of the ovary) and uncommonly other blood-containing lesions (e.g. haemorrhagic corpus luteum cysts).
The sign is seen on T2-weighted sequences of lesions that are hyperintense on T1, and consists of low signal (T2 shortening) affecting variable portions of the cyst. It may involve only a small portion of the cysts, typically layering dependently. Alternatively, it may involve the entire cyst. The signal is due to the high concentration of protein and iron within the endometrioma from recurrent haemorrhage. The degree of shading can vary from faint to complete signal loss.
There are different patterns of appearance 3:
homogenous shading: the most prevalent pattern in endometriomas
heterogeneous shading: the most specific for endometriomas
layering: the lower layers are darker
-
liquid–liquidfluid–fluid level: the least common
focal/multifocal shading within a complex mass: unlikely for endometriomas
Marked loss of signal intensity on T2-weighted images is not usually seen with haemorrhagic cysts, since they do not repeatedly bleed. Without recurrent haemorrhage and concentration of contents, the viscosity of the cyst remains lower, and shading is not present or less dark 1.
When noted with endometriosis, lesions demonstrating a shading sign may be less likely to respond to medical treatment 2.
History and etymology
It was first described by Nishimura and his team et al. in 19871987 4.
See also
-<p><strong>Shading sign</strong> is an MRI finding typically seen in an <a href="/articles/endometrioma">endometrioma</a>. It may also be seen with some endometrioid tumours (e.g <a href="/articles/endometrioid-carcinoma-of-the-ovary">endometrioid carcinoma of the ovary</a>) and uncommonly other blood-containing lesions (e.g. <a title="Haemorrhage into a corpus luteum cyst" href="/articles/haemorrhagic-corpus-luteal-cyst">haemorrhagic corpus luteum cysts</a>).</p><p>The sign is seen on T2-weighted sequences of lesions that are hyperintense on T1, and consists of low signal (T2 shortening) affecting variable portions of the cyst. It may involve only a small portion of the cysts, typically layering dependently. Alternatively, it may involve the entire cyst. The signal is due to the high concentration of protein and iron within the endometrioma from recurrent haemorrhage. The degree of shading can vary from faint to complete signal loss.</p><p>There are different patterns of appearance <sup>3</sup>:</p><ul>-<li>homogenous shading: the most prevalent pattern in endometriomas</li>-<li>heterogeneous shading: the most specific for endometriomas</li>-<li>layering: the lower layers are darker</li>-<li>liquid–liquid level: the least common</li>-<li>focal/multifocal shading within a complex mass: unlikely for endometriomas</li>-</ul><p>Marked loss of signal intensity on T2-weighted images is not usually seen with haemorrhagic cysts, since they do not repeatedly bleed. Without recurrent haemorrhage and concentration of contents, the viscosity of the cyst remains lower, and shading is not present or less dark <sup>1</sup>.</p><p>When noted with <a href="/articles/endometriosis">endometriosis</a>, lesions demonstrating a shading sign may be less likely to respond to medical treatment <sup>2</sup>.</p><h4>History and etymology</h4><p>It was first described by <strong>Nishimura</strong> and his team in <strong>1987 </strong><sup>4</sup>.</p><h4>See also</h4><ul><li><a title="T2 dark spot sign (endometrioma)" href="/articles/t2-dark-spot-sign-endometrioma">T2 dark spot sign (endometrioma)</a></li></ul>- +<p><strong>Shading sign</strong> is an MRI finding typically seen in an <a href="/articles/endometrioma">endometrioma</a>. It may also be seen with some endometrioid tumours (e.g. <a href="/articles/endometrioid-carcinoma-of-the-ovary">endometrioid carcinoma of the ovary</a>) and uncommonly other blood-containing lesions (e.g. <a href="/articles/haemorrhagic-corpus-luteal-cyst" title="Haemorrhage into a corpus luteum cyst">haemorrhagic corpus luteum cysts</a>).</p><p>The sign is seen on T2-weighted sequences of lesions that are hyperintense on T1, and consists of low signal (T2 shortening) affecting variable portions of the cyst. It may involve only a small portion of the cysts, typically layering dependently. Alternatively, it may involve the entire cyst. The signal is due to the high concentration of protein and iron within the endometrioma from recurrent haemorrhage. The degree of shading can vary from faint to complete signal loss.</p><p>There are different patterns of appearance <sup>3</sup>:</p><ul>
- +<li><p>homogenous shading: the most prevalent pattern in endometriomas</p></li>
- +<li><p>heterogeneous shading: the most specific for endometriomas</p></li>
- +<li><p>layering: the lower layers are darker</p></li>
- +<li><p>fluid–fluid level: the least common</p></li>
- +<li><p>focal/multifocal shading within a complex mass: unlikely for endometriomas</p></li>
- +</ul><p>Marked loss of signal intensity on T2-weighted images is not usually seen with haemorrhagic cysts since they do not repeatedly bleed. Without recurrent haemorrhage and concentration of contents, the viscosity of the cyst remains lower, and shading is not present or less dark <sup>1</sup>.</p><p>When noted with <a href="/articles/endometriosis">endometriosis</a>, lesions demonstrating a shading sign may be less likely to respond to medical treatment <sup>2</sup>.</p><h4>History and etymology</h4><p>It was first described by Nishimura et al. in 1987<strong> </strong><sup>4</sup>.</p><h4>See also</h4><ul><li><p><a href="/articles/t2-dark-spot-sign-endometrioma" title="T2 dark spot sign (endometrioma)">T2 dark spot sign (endometrioma)</a></p></li></ul>
Image 1 MRI (T2) ( update )

Image 2 MRI (T2) ( update )
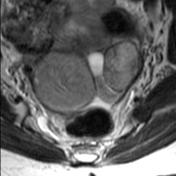
Image 3 MRI (T2 fat sat) ( update )

Image 4 MRI (T2) ( update )

Image 5 MRI (T2) ( update )
