Spinal nerve sheath tumors are the most common intradural extramedullary masses.
This article is an overview of spinal nerve sheath tumors. For a discussion on the epidemiology, clinical presentation, pathology and treatment/prognosis of spinal schwannomas and neurofibromas, please refer to spinal schwannoma and spinal neurofibroma.
On this page:
Epidemiology
Associations
35-45% of patients with nerve root tumors have neurofibromatosis 2. Multiple lesions are common in these patients. Neurofibromas are associated with NF1, whereas schwannomas are associated with NF2.
Pathology
Spinal nerve sheath tumors include, in order of decreasing frequency:
spinal schwannoma (30% of all intradural extramedullary lesions 6 and 65% of intradural extramedullary nerve sheath tumors 7)
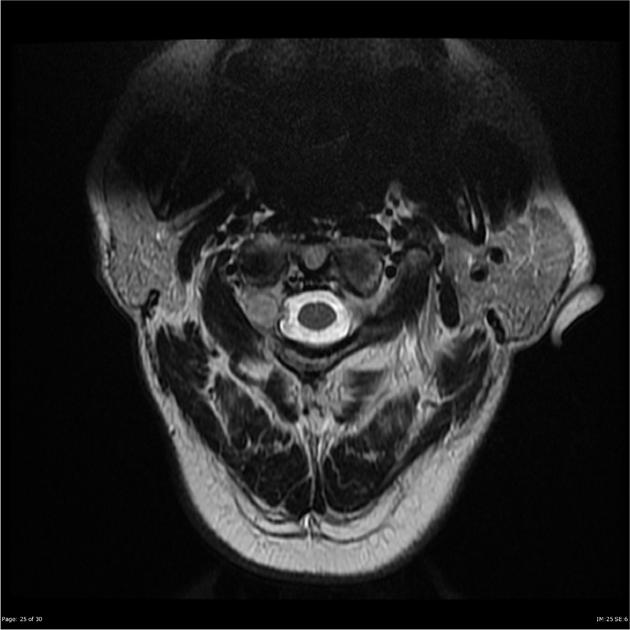
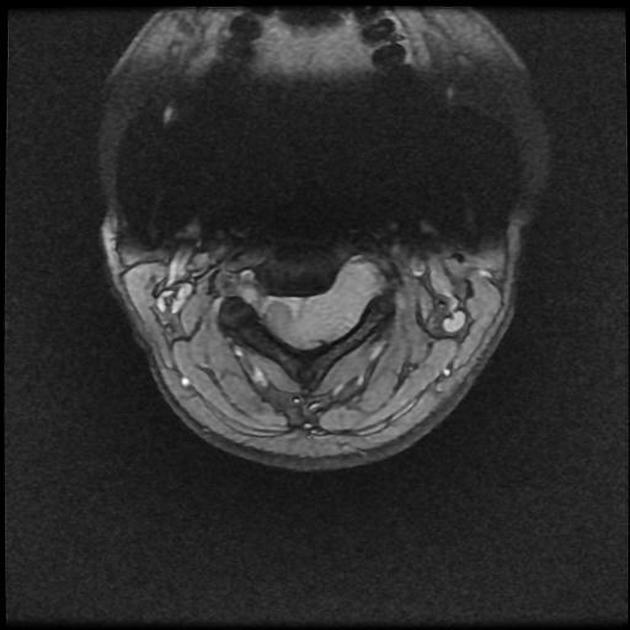
Most nerve sheath tumors arise from the dorsal sensory roots. 70% are intradural extramedullary in location, 15% are purely extradural and a further 15% have both intradural and extradural components (“dumbbell” lesions). Less than 1% are intramedullary 2.
Radiographic features
Schwannomas and neurofibromas are often indistinguishable radiographically.
Plain radiograph
Bone changes can be common on plain film and can include:
enlarged neural foramina
pedicle erosion
CT
density varies from hypodense to slightly hyperdense
widened neural exit foramina
bone erosion
paraspinous soft tissue mass: “dumbbell” and extradural lesions
calcification and hemorrhage are rare
MRI
Schwannomas are frequently associated with hemorrhage, intrinsic vascular changes (thrombosis; sinusoidal dilatation), cyst formation and fatty degeneration. These findings are rare in neurofibromas 4.
Neurofibromas tend to encase the nerve roots, in contrast to schwannomas which commonly displace the nerve root due to their asymmetric growth.
Schwannomas are usually round, whereas neurofibromas are more commonly fusiform.
T1: 75% are isointense, 25% are hypointense 2
-
T2: >95% are hyperintense 2
schwannomas may have mixed signal intensity on T2
a hyperintense rim and central area of low signal resulting in a target sign may be seen in neurofibromas and occasionally also in schwannomas; this is thought to be due to a dense central area of collagenous stroma
-
T1 C+ (Gd)
virtually 100% enhance
heterogenous enhancement with areas of low signal is more characteristic of a neurofibroma
Differential diagnosis
-
broad dural base
usually located posterolaterally (compared to nerve sheath tumors which are typically located anteriorly)
neural exit foraminal widening is less commonly seen with meningiomas than with nerve sheath tumors
-
usually seen as a well-circumscribed mass inferior to the conus
flow voids are typically seen along the surface of and within the tumor nodule
hemorrhage is common, leading to a "cap sign" on T2 weighted images
the characteristic “salt-and-pepper” appearance of neck and skull base paragangliomas may be seen
-
occur almost exclusively in the conus medullaris and filum terminale
hemorrhage is common
-
intradural extramedullary metastases
an important differential for multiple neurofibromas
cord edema may be seen with more extensive disease, especially if there is an intramedullary component
“sugar coating” of the spinal cord and nerve roots may be seen
-
perineural root sleeve cyst
CSF density on CT; CSF intensity on T1 and T2 weighted images
no contrast enhancement
-
-
epidermoid
similar intensity to CSF on T1 and T2 weighted images
typically non-enhancing, however, a thin rim of contrast enhancement may be seen
diffusion restriction on DWI
-
dermoid
presence of fat is suggestive
usually present in younger patients (<20 years)
associated dermal sinus may be present
-
-
intradural disc herniation
no enhancement




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.