Spinal subdural haematomas (SSDH) are much less common than epidural haematomas; however, progression of symptoms due to compression tends to be faster 1.
On this page:
Epidemiology
Spinal subdural haematomas are a rare entity, much more so than epidural haematomas. In a meta-analysis of over 600 spinal haematomas, only 4% were subdural 2.
Clinical presentation
Symptoms are those of spinal cord compression or cauda equina syndrome, often presenting initially as back pain and/or radicular pain. Symptoms tend to develop more rapidly with subdural haematomas.
Pathology
Aetiology
Factors that predispose to subdural haematoma include:
coagulopathy
anticoagulant therapy 3,4
percutaneous spinal intervention 5
back surgery 6,7
trauma 8: uncommon cause
a combination of any of the above
Radiographic features
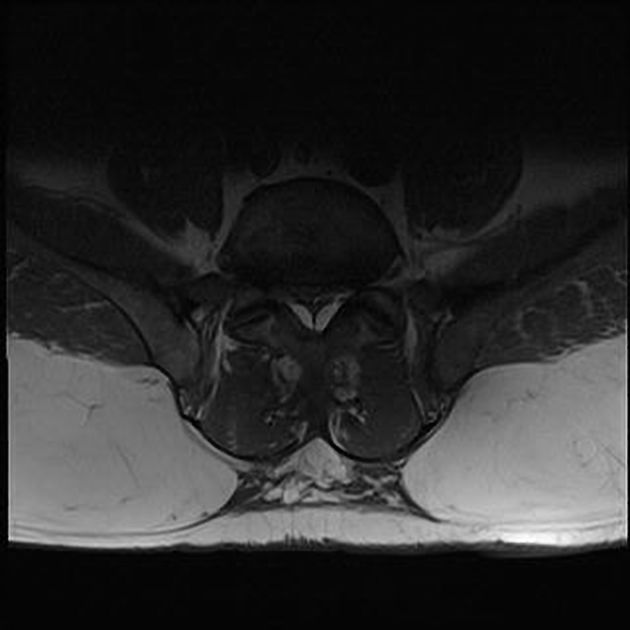
Subdural haematomas occur within the dural sac; therefore, in contradistinction to epidural haematomas, the epidural fat is preserved and the dura is not displaced inward. The haematoma is bounded by the paired lateral denticulate ligaments and the dorsal septum, forming the inverted Mercedes-Benz sign on axial images 1. As such, it compresses the nerve roots but does not extend into the neural foramina or make direct contact with bone. Naturally, smaller collections will not expand the potential subdural space and will, therefore, not create the inverted Mercedes-Benz sign.
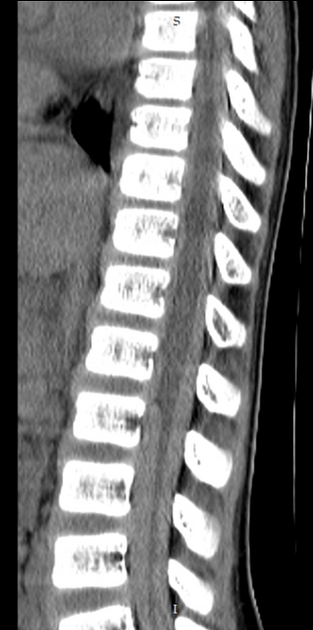
CT
A crescentic hyperdense collection may be seen adhering to the inner margin of the dura, separated from the hypodense epidural fat.
These CT findings may be subtle. Use of a narrow window setting can help identify a haematoma. CT can also sometimes help clarify the haematoma aetiology 1.
MRI
MRI is the imaging modality of choice for identifying and characterising subdural haematomas.
Signal characteristics will vary, depending on the age of the blood.
After having confirmed the location of the collection as subdural on axial images, sagittal images can be utilised for measuring its extent.
Treatment and prognosis
Conservative treatment with watchful waiting (i.e. follow-up with serial MRIs) is acceptable for small collections. In case of significant neurologic defects, laminectomy with clot evacuation is done.
Cervical and thoracic SSDH are associated with a worse outcome than lumbar SSDH, as is coexisting spinal subarachnoid haematoma (SSAH).
Differential diagnosis
It is important to distinguish between subdural haematomas and other entities which can occupy the spinal subdural space:
-
subdural empyema: rare
different history and clinical picture, including fever
local extension or haematogenous spread, or iatrogenic
behaves differently on MRI
-
subdural hygroma: CSF collection
appears as clumping of nerve roots in shape of inverted Mercedes-Benz sign
injury to dura mater may be directly detected
-
large hygroma can show MRI signs of craniospinal hypotension:
spinal epidural haematoma: there is absence of the epidural fat stripe between the blood collection and spinal canal
epidural lipomatosis: fat-sat sequences will help differentiation between early subacute SSDH and lipomatosis
intradural-extramedullary mass: meningiomas and nerve sheath tumours (both common) enhance avidly, while arachnoid cysts follow CSF signal on all sequences
arachnoiditis: nerve root clumping surrounded entirely by CSF (i.e. not the inverted Mercedes-Benz appearance)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.