Status epilepticus is an acute and prolonged seizure that persists for a sufficient length of time or is repeated frequently enough that recovery between attacks does not occur. It is a clinical emergency associated with high morbidity and mortality.
On this page:
Terminology
Status epilepticus is a broad term that encompasses prolonged seizures. Additional qualifiers to 'status epilepticus' may be used in treatment-refractory cases 11:
refractory status epilepticus: when first- and second-line treatments (including one non-benzodiazepine) have failed
super-refractory status epilepticus: when status epilepticus has continued or recurred despite therapy with general anaesthesia for 24 hours or more
Epidemiology
The estimated incidence of ~35 per 100,000, and it is more common in lower socioeconomic populations 1.
Clinical presentation
Although the definition of status epilepticus proposed by the International League Against Epilepsy (ILAE) does not provide a definite time-frame, the ILAE suggested operational time-frames after which a seizure will likely become continuous 8:
tonic-clonic status epilepticus: 5 minutes
focal status epilepticus with impaired consciousness: 10 minutes
absence status epilepticus: 15 minutes
Broad clinical categories of status epilepticus include 8,10:
convulsive status epilepticus (CSE): presence of prominent motor features which may be either focal or generalised (or unknown) at onset
nonconvulsive status epilepticus (NCSE): absence of prominent motor features which is often caused by absence status epilepticus or focal with impaired consciousness status epilepticus
Pathology
In patients with a known history of seizures, common causes of a status epilepticus are changes in antiseizure medications or withdrawal syndrome. Approximately 50% of these events occur in patients without any history of epilepsy and are usually related to an underlying condition, such as 1,2:
hypoxia
metabolic derangement (e.g. hypoglycaemia)
toxicity (e.g. drugs)
encephalitis
alcohol intoxication or withdrawal
pregnancy-related (e.g. eclampsia)
infections accompanied by fever (the most important cause in children)
Radiographic features
CT
In most instances, unless one of the underlying conditions is visible (e.g. stroke), CT of the brain will be unremarkable.
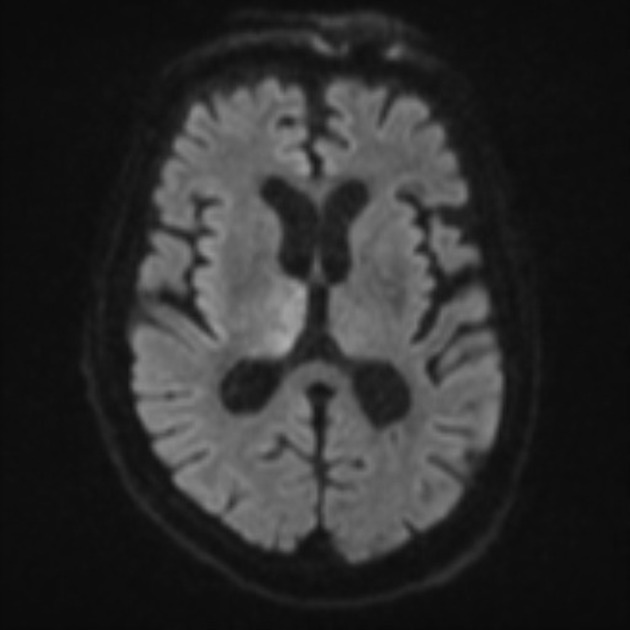
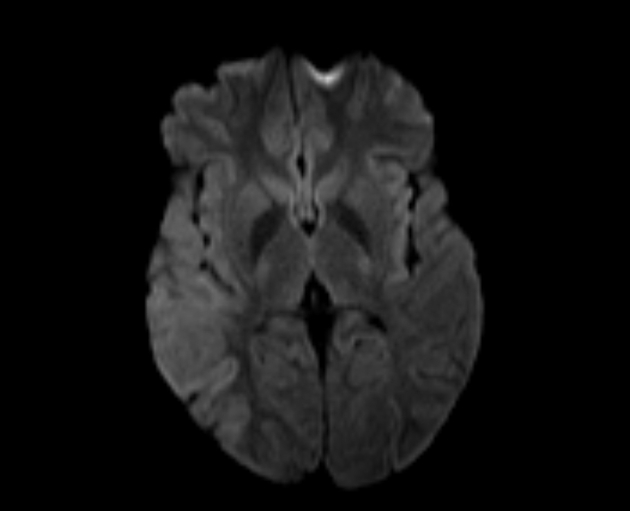
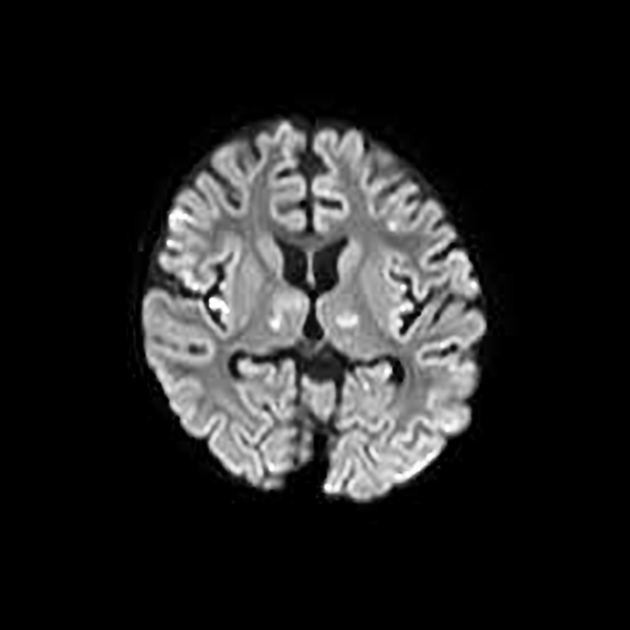
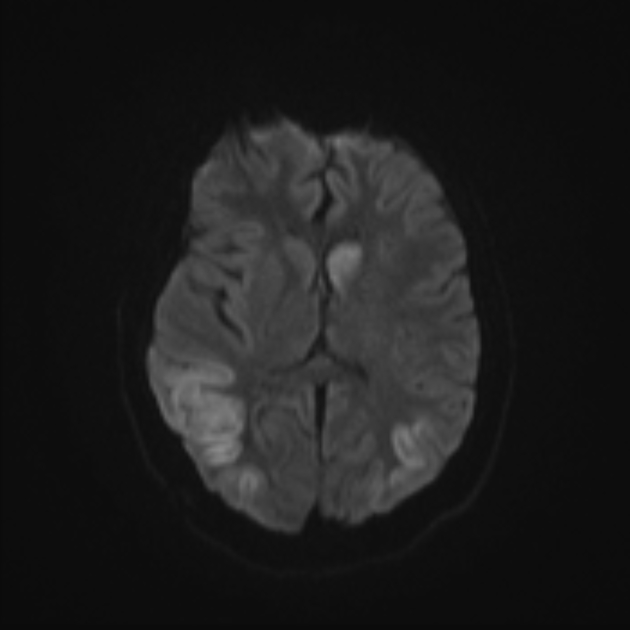
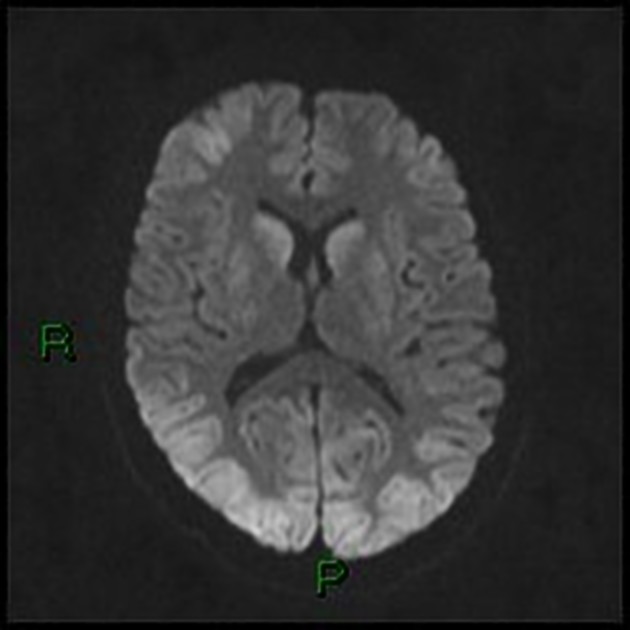
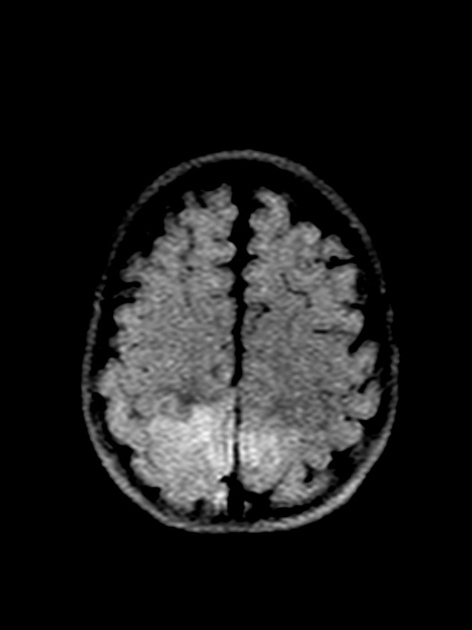
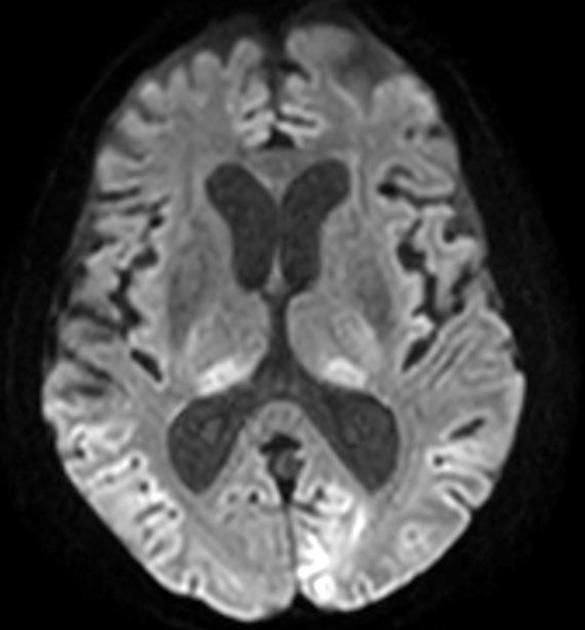
MRI
The most common changes seen relate to an increased T2 signal (best seen on FLAIR) with some swelling. These regions may demonstrate corresponding diffusion abnormalities, with increased DWI signal and in some instances reduced ADC values 3,6. These changes are believed to be due to excessive metabolic demands placed on tissues due to sustained seizure activity, resulting in vasogenic and/or cytotoxic oedema. If severe enough, cell metabolism will fail resulting in eventual cell death 3,4.
It is important to note that diffusion needs to be assessed on ADC maps and not DWI as it is not possible to confidently distinguish true diffusion restriction from T2 shine through on DWI images only. When T2 signal elevation is associated with significant (>10%) drop in ADC values, follow-up is likely to reflect permanent damage 3,6. In contrast, isolated T2 signal change, without ADC signal drop is likely to fully resolve 3.
Post-contrast T1 imaging is extremely variable, ranging from no enhancement to marked enhancement, which may be gyriform or leptomeningeal in distribution.
The locations involved are variable, including 3,5:
cerebral cortex and subcortical white matter
hippocampi and mesial temporal lobes
thalamus, particularly the pulvinar region 5
Treatment and prognosis
Management is complex and many institutions will have their own treatment algorithms or protocols. Broad principles include 12:
first aid
-
initiation of antiseizure medications
first-line: benzodiazepine
second-line: loading dose(s) of other non-benzodiazepine antiseizure medications (e.g. levetiracetam, sodium valproate, phenytoin, lacosamide, etc.)
third-line: intubation with antiseizure medication and/or anaesthetic infusion(s) (e.g. midazolam, propofol, thiopentone, ketamine, phenobarbital, etc.)
concurrent management of the underlying cause if known and if possible
Differential diagnosis
functional seizures (previously, psychogenic non-epileptic seizures)





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.