Sural neuropathy, also known as sural nerve entrapment, can be the result of nerve compression or traction injury of the sural nerve. This nerve is a purely sensory branch, usually formed by a confluence of branches from the tibial nerve and common peroneal nerve that supplies the lateral aspect of the ankle and the foot to the base of the fifth toe 1,2.
On this page:
Epidemiology
Associations
Sural nerve entrapment is usually associated with traumatic injuries 1-3.
Diagnosis
The diagnosis is usually made on clinical grounds and if this is difficult can be confirmed with electrodiagnostic tests like nerve conduction studies. Differential diagnoses, such as common peroneal nerve, tibial nerve entrapment and radiculopathy should be ruled out. A diagnostic sural nerve block is another option to confirm the diagnosis. Imaging studies, such as MRI, might help to identify the location of the entrapment and provide clues about the aetiology 1.
Clinical presentation
Presenting symptoms include pain and paraesthesia along the lateral aspect of the foot and ankle including the base of the fifth toe 1,3 which might be exacerbated by plantar flexion and/or inversion of the foot 2. Chronic calf pain exacerbated by physical activity is another symptom 2. A positive Tinel sign or point tenderness at the entrapment site might be another clinical clue.
Pathology
Sural nerve neuropathy can be a result of an acute traumatic injury at different sites, chronic compression due to tendon dislocation or entrapment within a scar 4 or as a consequence of a traction injury with secondary fibrosis 2,3.
Aetiology
The cause is usually related to a traumatic injury affecting the sural nerve including 1-4:
direct contusion
distal fibular fracture, talar, calcaneal or cuboid fracture
severe lateral ankle sprain
gastrocnemius injury
space-occupying lesions
iatrogenic injury (surgery)
Location
Sural neuropathy due to a direct traumatic event can happen at multiple different sites along its course 1-3. A common location is at the level of the fifth metatarsal base where it bifurcates into its medial and lateral terminal branches 2,3. Another potential site would be the lateral aspect of the calf where the sural nerve leaves the crural fascia 5.
Radiographic features
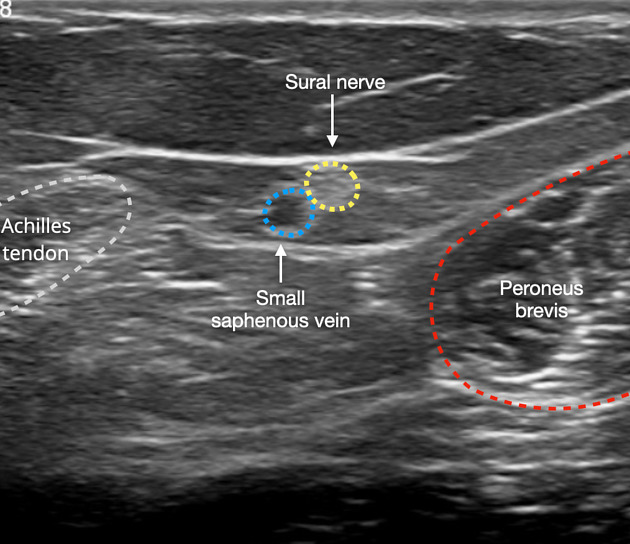
Ultrasound
In the calf, the sural nerve can be visualised on top of the gastrocnemius muscle at a midcalf level and descends with the small saphenous vein 6,7. Further distally it may be seen between the Achilles tendon and the peroneal muscles and below or posterior to the peroneal tendons and superficial to the peroneal retinacula and the calcaneofibular ligament at the level of the calcaneus 6,7.
In sural nerve neuropathy, the nerve might be thickened and hypoechoic with partial or complete loss of its normal fascicular pattern 7. Local compression with the ultrasound probe might reproduce pain and ultrasound can be utilised for the guidance of a diagnostic nerve block 7.
MRI
MRI might visualise displacement or compression of the sural nerve due to traumatic injury or space-occupying lesions 2. Since the sural nerve is pure sensory there will not be any denervation changes 2.
Radiology report
The radiology report should include a description of the following 6:
abnormal appearance of the sural nerve and location
neuroma formation
associated underlying pathology
Treatment and prognosis
Management includes conservative measures including physiotherapy, local anaesthetics, nonsteroidal anti-inflammatory drugs. Surgery might be required for the removal of space-occupying lesions and involves decompression and neurolysis 5.
History and etymology
Some of the first reported cases of sural nerve neuropathy were described by R Pringle and colleagues in 1974 4,8.
Differential diagnosis
The differential diagnosis of superficial sural nerve entrapment includes:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.