Tenosynovitis is a term describing the inflammation of the synovial membrane surrounding a tendon. It may be seen with or without tendinosis/tendinitis. The synovial membrane is part of a fluid-filled sheath that surrounds a tendon.
On this page:
Clinical presentation
joint swelling
pain in the affected area
pain/grating sensation when moving the affected joint
difficulty moving a joint
erythema along the length of the affected tendon
Pathology
Aetiology
Tenosynovitis can be caused by a variety of disease processes, including, but not limited to:
trauma/injury
mechanical irritation
rheumatoid arthritis: most common to involve extensor carpi ulnaris and flexor carpi radialis
Subtypes
-
hypertrophy of the flexor pulley: trigger finger
flexor hallucis longus in patients with os trigonum syndrome
Radiographic features
Plain radiograph
Plain radiographs are non-diagnostic but may show calcification of one or several synovial membranes (suggestive of hydroxyapatite deposition/chondrocalcinosis) and a periosteal reaction in an adjacent bone.
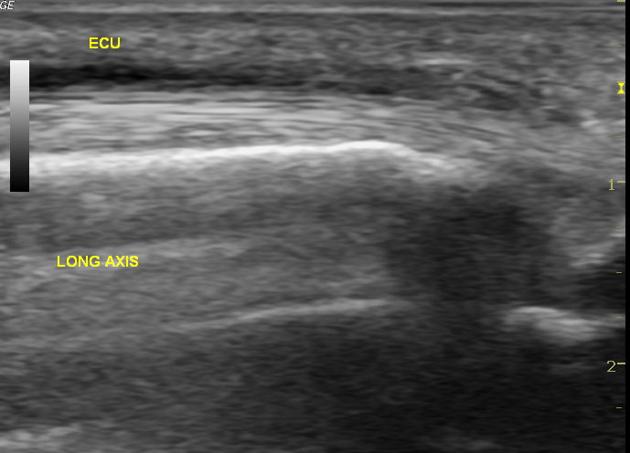
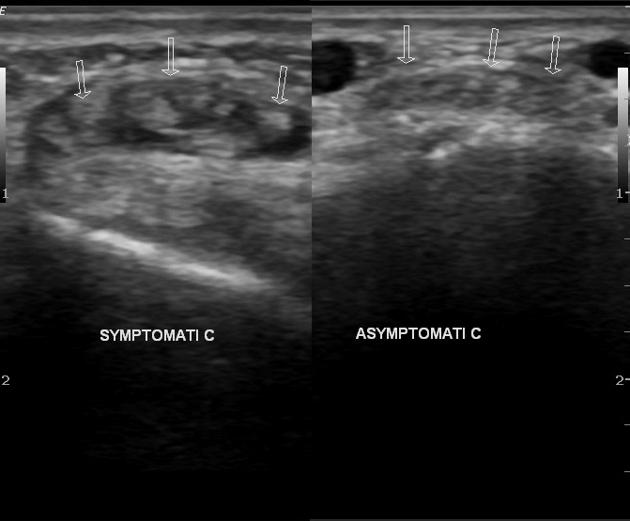
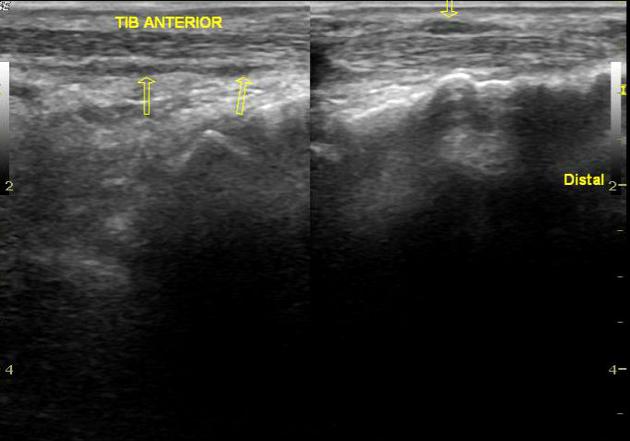
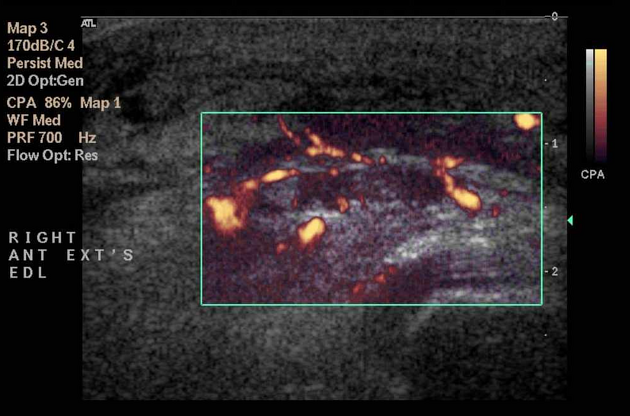
Ultrasound
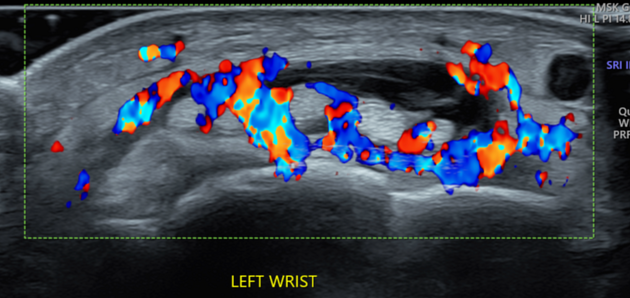
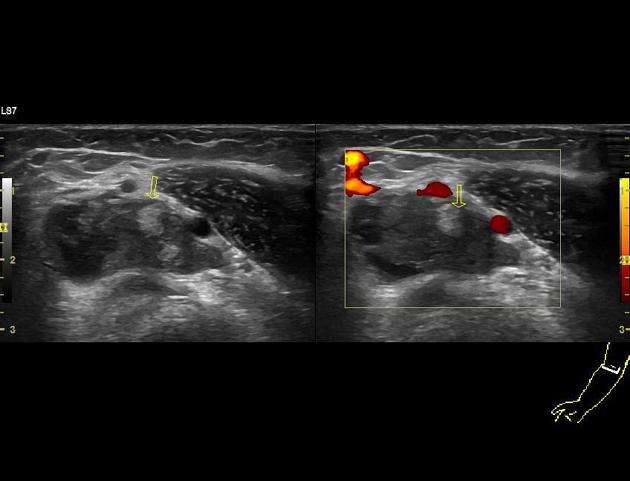
The synovial membrane is not identified unless there is a pathological swelling. Tenosynovitis is characterised by increased fluid content within tendon sheath, thickening of the synovial sheath with or without increased vascularity which can extend into the tendon sheath, and peritendinous subcutaneous oedema. Subcutaneous oedema can result in a hypoechoic halo sign and peritendinous subcutaneous hyperaemia on Doppler imaging.
Colour Doppler ultrasound is an important part of the tendon sheath assessment; it can differentiate between synovial thickening which is more suggestive of chronic disease, and turbid tendon sheath fluid collection - more indicative of acute exudative tenosynovitis. In chronic inactive disease, however, there is synovial thickening with minimal vascularity.
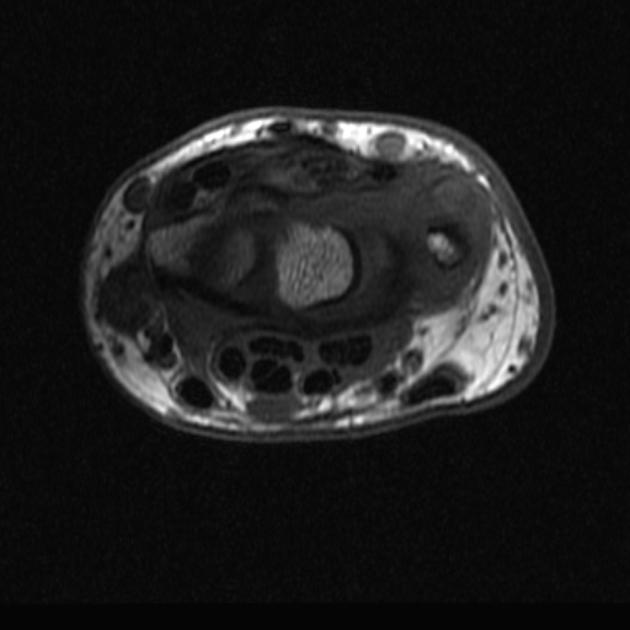
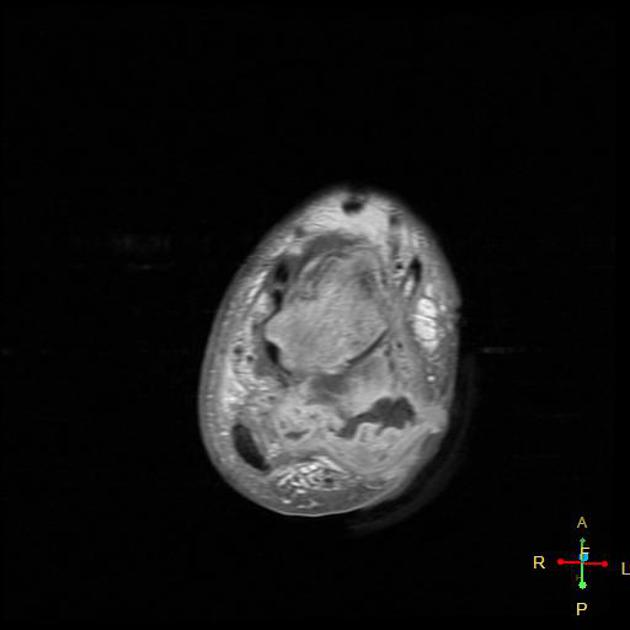
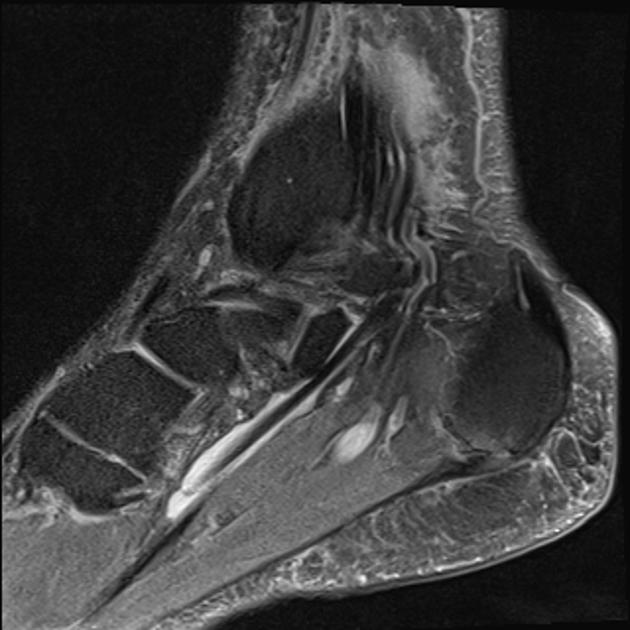
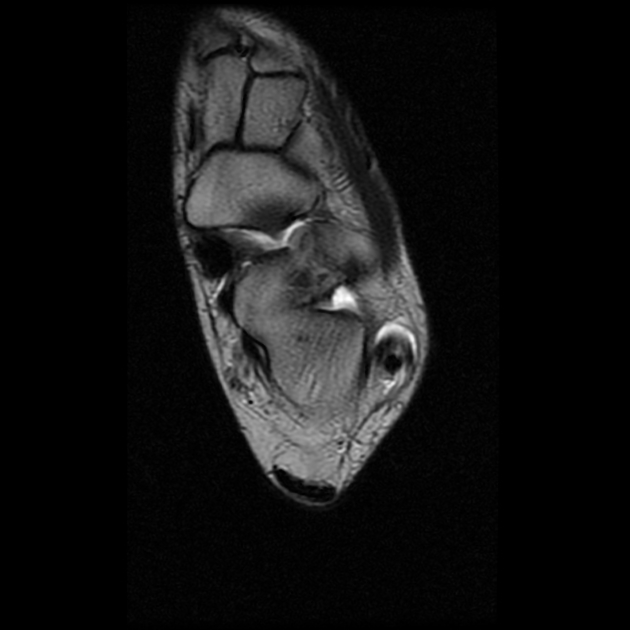
MRI
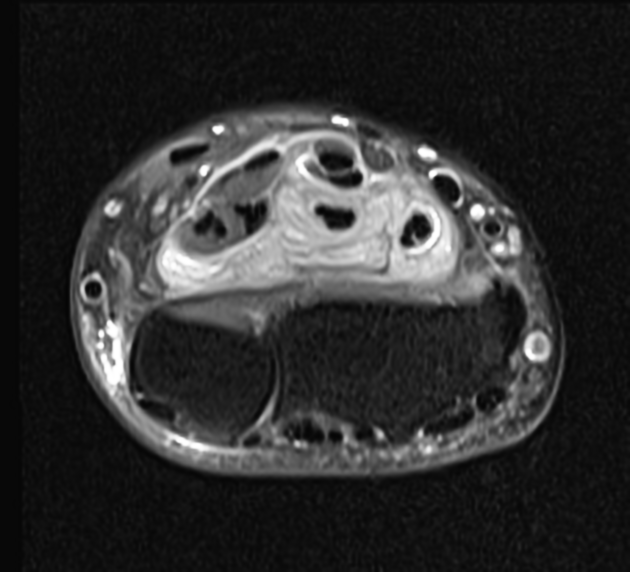
Increased fluid within tendon sheath:
T1: low or intermediate if debris within tendon sheath
T2: high
T1 C+ (Gd): tendon sheath thickening and peritendinous subcutaneous contrast enhancement
Treatment and prognosis
Treatments may include activity modification, rest, non-steroidal anti-inflammatory drugs, bandage or splint, and/or cold therapy. Surgical procedures to release the tendon rarely have a role. If tenosynovitis persists after a period of rest and infection has been excluded, a steroid injection may provide symptomatic relief. If the tenosynovitis is infective, urgent surgical assessment is required. Physiotherapy is an option.
Practical points
If the tendon communicates with a joint, such as the long head of biceps at the shoulder and flexor hallucis longus at the ankle, then no fluid should be present in the joint to make the call.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.