Selective transcatheter arterial embolisation (TAE) of renal angiomyolipomas (AML) is a minimally invasive treatment of renal angiomyolipomas. It is appealing because it can save a significant part of the normal renal parenchyma despite tumour embolisation with a superselective approach and subsequent few post-operative complications 1.
On this page:
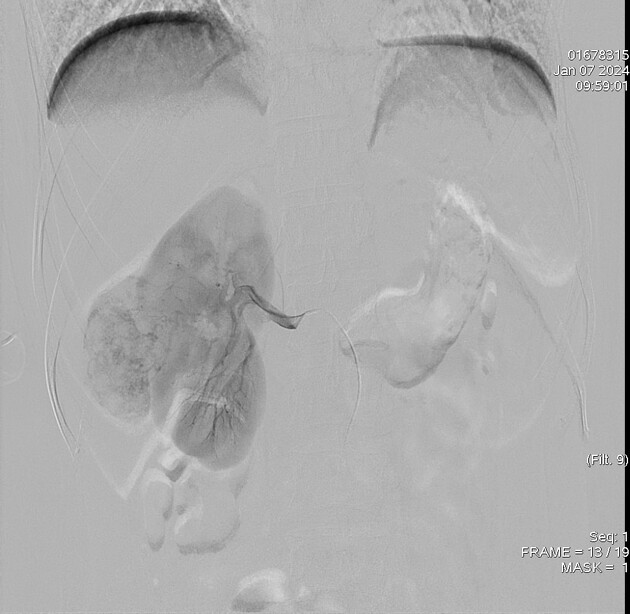
Images:
Indications
ruptured renal angiomyolipoma with haemorrhage
symptomatic cases with flank pain/mass effect
renal AML > 4 cm which may have microaneurysms as an early warning sign of increased risk of rupture
prevention of major bleeding during pregnancy
Contraindications
acute infection: to prevent abscess in the targeted area
impaired global renal function (eGFR<35)
allergic reactions to contrast media
acute hyperthyroidism
single kidney
Procedure
Technique
trans-femoral access
selective cannulation of the main renal artery
superselective angiogram from the renal artery branch supplying the tumour
preparing of ethanol-lipiodol mixture in 1:1 or 2:1 depending on the position of the microcatheter, vascularity, and flow (or we can use PVA, Glue, or Coils)
start with very small volumes of the mixture (2 mL) and then extreme care and patience during the injection
avoid reflux and nontarget embolisation of mixture into normal branches
the endpoint of embolisation can arrive very abruptly
final main renal artery angiogram
prophylactic antibiotics 2,5
Complications
-
post embolisation syndrome (PES)
fever (above 38.0°C), nausea, and abdominal pain
minimal swelling and discomfort around the catheter site
renal abscess
thrombosis of the renal artery
complete loss of renal function (rarely)
TAE may not lead to a full response
Outcome
Transcatheter arterial embolisation is considered an alternative treatment choice for renal AMLs and the literature indicates that the TAE technique has significantly reduced median tumour size, with a low incidence of severe complications and no notable loss of renal function during long-term follow-up. In particular it may be considered in patient cases who are not candidates for abdominal surgery 1-5.
Advantages
the procedure can be carried out in an outpatient setting using local anaesthesia
non-invasive and more nephron-sparing option than surgery
shrinkage of the mass over time
relieve symptoms caused by tumour pressure affecting nearby tissues
reducing the risk of internal bleeding
an alternative treatment option for patients who are not suitable for general anaesthesia, have a history of previous abdominal surgery or are at high risk of surgical complications due to other comorbidities 1,2
Disadvantages
no histological information is obtained, and renal cancer could potentially be missed 1,2





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.