Presentation
Chronic recurrent pancreatitis with liver abscesses, and markedly elevated CRP. Phyiscal exam suggestive of ascites.
Patient Data





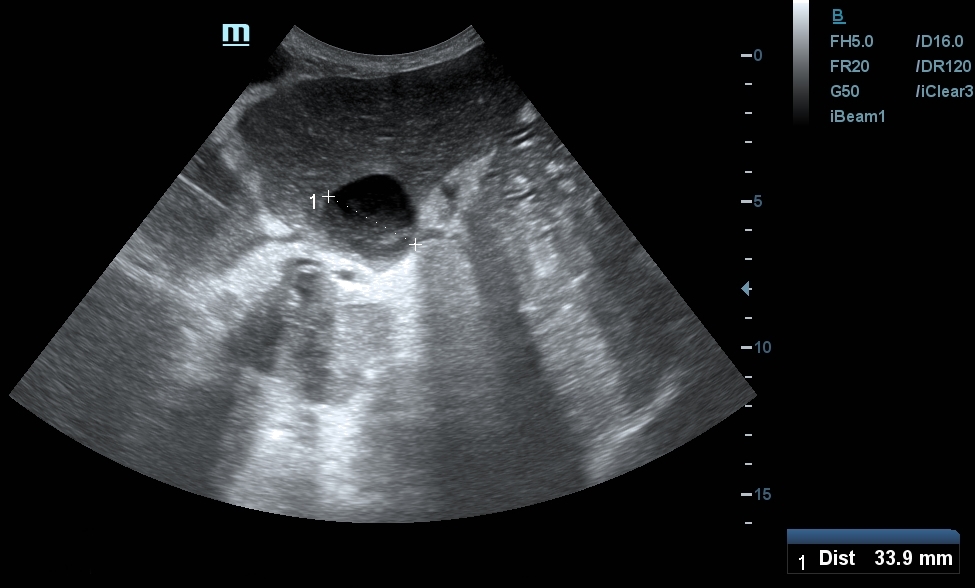
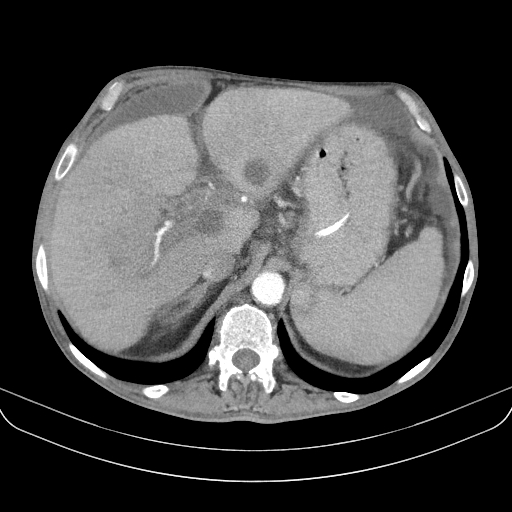
- multiple complex fluid-filled cystic abnormalities in the liver suggestive of abscesses
- significant amount of free fluid in the pelvis, septated complex free fluid adjacent to the liver
- portal vein can not be identified, instead meandering venous branches are visible in the porta hepatis, indicating portal vein thrombosis and consequent cavernous transformation
The cavernous transformation can be better appreciated in the cine loop.


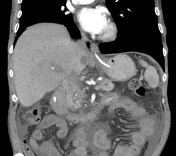



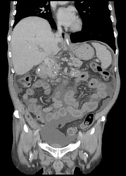

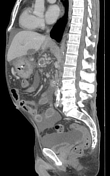

CT provided for explanation:
- significant amount of intraperitoneal free fluid
- multiple cystic lesions in the liver containing relatively low density fluid - most likely represent abscesses
- portal vein is occluded, cavernous portal transformation is striking. Well-developed collateral veins
- inhomogenous, atrophied pancreas with surrounding diffuse fat stranding representing chronic pancreatitis, marked dilation of the pancreatic duct
- hypodense gastric antral and duodenal wall, possibly due to inflammation
- other unrelated findings: gallstone, chronic kidney disease, bilateral adrenal hyperplasia
Case Discussion
Typical presentation of chronic portal vein thrombosis with cavernous transformation of the porta hepatis that developed as a complication of chronic pancreatitis. This pathology has a striking, characteristic appearance on ultrasound, but can be easily missed if color Doppler is not applied. In a similar scenario, the presence of a newly developed ascites is an alarming feature that warrants careful scrutiny of the portal venous flow.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.