Presentation
Known Waldenstrom's macroglobulinaemia. A biopsy of nasal mucosa showed granulomas.
Patient Data






















The nasal mucosa is slightly prominent and hyper-enhancing, particularly on the left, but not more so than is often seen. No nodularity or perforation is evident. The paranasal sinus mucosa is similarly slightly thickened.
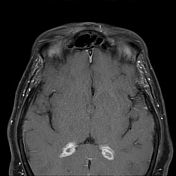
More convincing and concerning is dural thickening of the tentorium as well as in the posterior fossa and along the falx. The choroid plexus is hyperenhancing with adjacent subependymal oedema. No hydrocephalus. Probable leptomeningeal enhancement.
Extensive thick nodular enhancement is also seen around both optic nerves, more pronounced on the left.
Diffuse low T1 signal marrow infiltration is best seen in the mandible, but is present in all visualised sekeltal elements.
Nasal septum biopsy
The stroma shows florid, non-necrotising granulomatous inflammation with well-developed collections of epithelioid histiocytes and scattered multinucleate giant cells. The granulomas do not have any significant lymphocyte cuffing, which is in keeping with sarcoidal-type granulomas. Features of polyarteritis nodosa or vasculitis are not seen. There is no evidence of malignancy. No bacteria or fungal elements are seen with Gram, GMS, Fite, Ziehl-Neelsen or PAS-D stains.
Diagnosis:
Non-necrotising granulomatous inflammation. Although a diagnosis of exclusion, the features are compatible with sarcoidosis in the appropriate context. Given the location of the lesion, granulomatosis with polyangiitis has been considered and cannot be definitively excluded, however the absence of tissue necrosis and vasculitis and the well-formed nature of the granulomas are against this diagnosis.
Lymph node biopsy (neck)
Core biopsies showing widespread sarcoidal granulomatous inflammation and fibrosis with background population of predominantly small mature lymphocytes and some plasma cells, polyclonal by IHC. There is no necrotising granulomatous inflammation and no overt lymphoid atypia. Special stains for fungal and acid-fast organisms are negative. A high proportion of the lymphocytes are small B cells, CD20, CD79a, PAX5 and IgM positive. There are scattered small dendritic meshworks and very occasional clusters of BCL6 positive/CD10 negative B cells, but no identifiable germinal centres on H&E. There is no CD20/CD5 co-expression. EBER ISH is negative. Ki-67 shows low activity (<10%).
Diagnosis:
Histopathology most likely in keeping with sarcoidosis; less likely granulomatosis with polyangiitis
Case Discussion
Discussion
Bone marrow infiltration is presumably due to Waldenstrom macroglobulinaemia.
Intracranial features are suspicious for pachymeningeal and choroid plexus involvement. In the setting of the neck and nasal biopsy histology, this likely represents involvement by a granulomatosis disease. In this instance, both granulomatosis with polyangiitis and sarcoidosis are possibilities.
Choroid plexitis is most commonly seen secondary to infection and usually is not the dominant feature.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.