Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS)
Presentation
A case of HLH post-BMT (since 2010) presented with dizziness, blurred vision, unsteady gait to rule out cerebral /cerebellar insult.
Patient Data
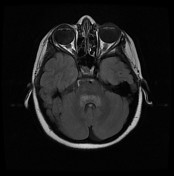



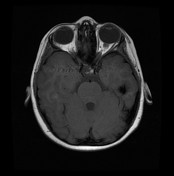

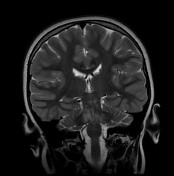

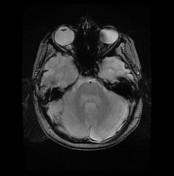

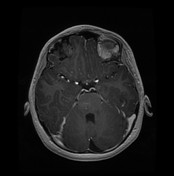



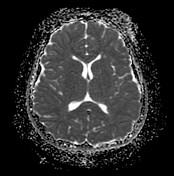

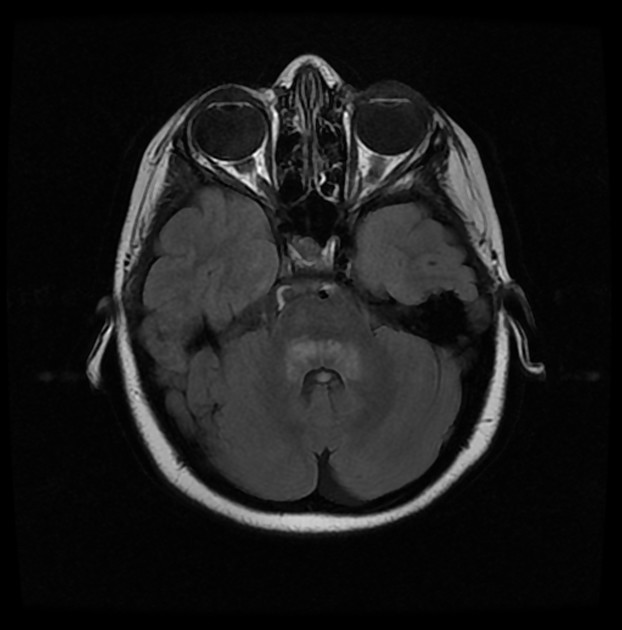
Patchy, confluent areas of the abnormal signal are seen implicating and the most posterior aspect of the pons (anterior to the 4th ventricle and as if capping it) as well as medial aspects of both middle cerebellar peduncles and related parts of cerebellar hemispheres. The lesions extend slightly down (caudally) to the upper medulla oblongata. Another fine nodule is seen anterior to the left aspect of the pons. The lesions appear iso to slight faint high signal on T1, bright on T2 & flair T2 with no blooming or diffusion restriction. On the post-contrast study, the lesion shows nonconfluent punctate curvilinear enhancement pepping into the pons. No mass effect exerted yet some swelling of the pons and middle cerebellar peduncles may be appreciated. In view of the patient history of Haemophagocytic Lymphohistiocytosis post-BMT, the possibility of Chronic Lymphocytic inflammation with pontine Perivascular enhancement responsive to steroids (CLIPPERS) may be considered as if pathogenesis not fully defined may spectrum of paediatric Demyelination autoimmune process. Another associated few scattered foci of high signals are seen within the periventricular white matter the more prominent ones in the left frontal region. No mass effect or perifocal oedema.
Case Discussion
In view of the patient history and MRI findings, the possibility of an autoimmune-mediated or inflammatory process as CLIPPERS is considered. Follow up after one week, we informed via the treating physician that the patient lesions almost resolved (The exam unfortunately performed in another hospital) The DD is less likely: Vasculopathy, demyelinating disorders, or neurosarcoidosis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.