Presentation
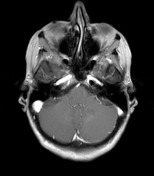
Progressive cerebellar ataxia and left arm ataxia. Previous MRI has showed a left middle cerebellar peduncle lesion. The patient had been diagnosed with MS and was previously followed with this diagnosis.
Patient Data
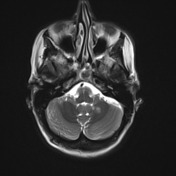




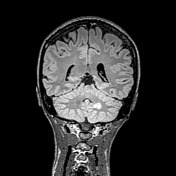



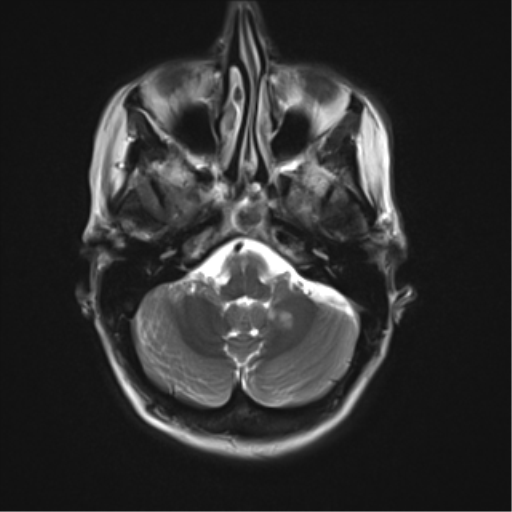
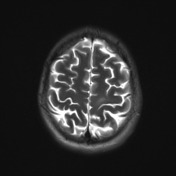
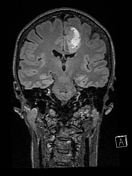
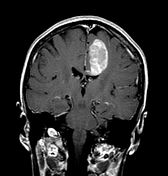
The mildly irregular heterogeneous hyperintense ovoid lesion centred medially in the left cerebellar hemisphere adjoining the middle cerebellar peduncle has remained stable in size and appearance when compared with the 6 months previous exam.
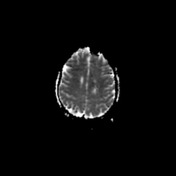
As previously, this demonstrates no overt pathologic enhancement and borderline diffusion restriction.
While the lesion may represent a demyelination plaque, ongoing follow-up MRI (including targeted spectroscopy) is recommended to exclude other lesions, such as a low-grade glioma.
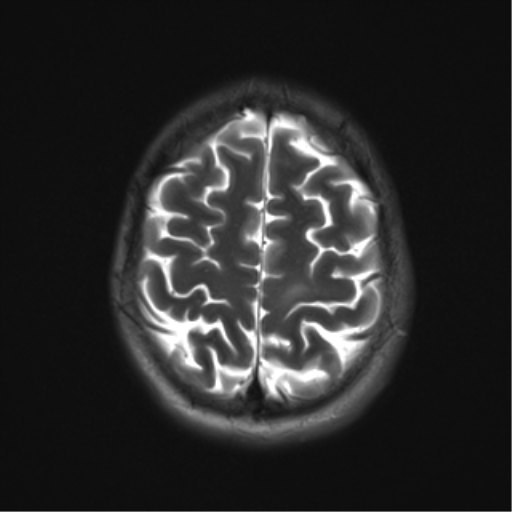
Interestingly, a very subtle ill-defined juxta-cortical lesion has also remained stable superiorly in the left precentral gyrus.
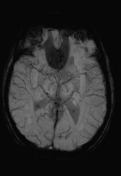
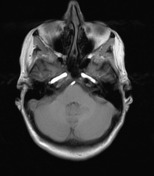
Multiple tiny ill-defined enhancing foci scattered elsewhere through the brain (including the right and left pons, right frontal lobe subcortical to deep white matter and anterior left caudate nucleus head) have also remained stable.
These are not associated with any overt T2 hyperintense signal abnormality and are thought most likely to represent multiple capillary telangiectasias.





Dizziness worse. New MRI 1 mth later to evaluate changes or progression.
No definite change allowing for technical differences. The left middle cerebellar peduncle FLAIR hyperintense T1 hypointense lesion is again noted together with the left precentral gyral lesion.
No definite new lesion allowing for artefact (marked artifact in the pons). No diffusion restricting or enhancing lesion apart from the subtle wispy areas of enhancement previously reported as capillary telangiectasiae. No progressive atrophy.
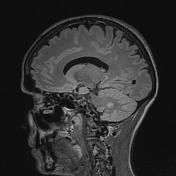
Stable previously reported pineal cyst.
IMPRESSION: No significant change or evidence of activity.
The patient was followed with periodic MRI scans during the next three years. All the exams during this period have shown lesions stability. The patient has was on Gilenya (sphingosine 1-phosphate (s1P) receptor modulator).
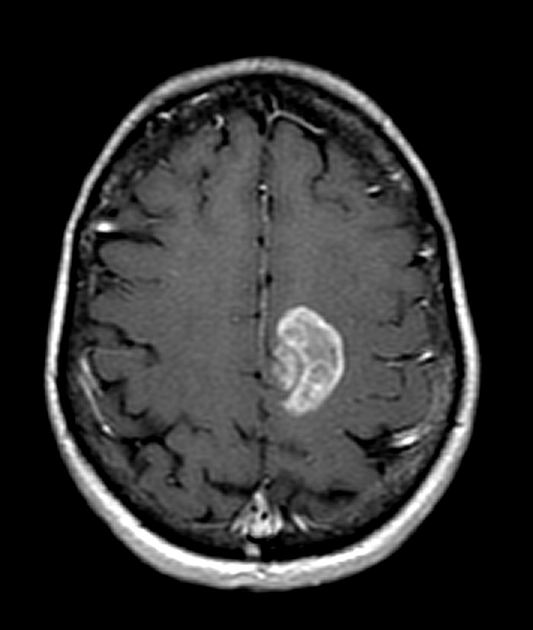
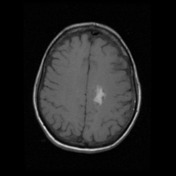
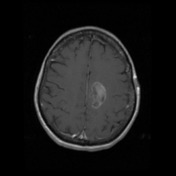
On a routine follow-up MRI scan, performed 5 years from the first exam shown above, a haemorrhagic mass was observed in the left frontal lobe. The cerebellar lesion and remaining features were stable. The patient did not show any new symptoms.

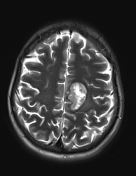
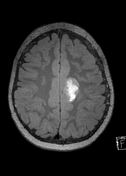
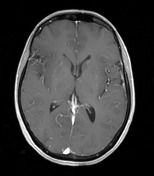
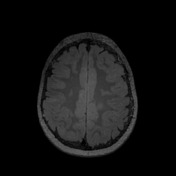
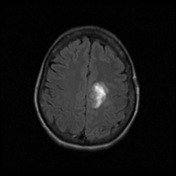
MRI images show a large new periventricular lesion that has developed since the previous examination, extending from the left body of corpus callosum and into the subcortical white matter of the left posterior frontal lobe. Although the position and perpendicular orientation to the lateral ventricle wall would fit with the stated history of multiple sclerosis, the lesion signal characteristics include heterogeneous T1 and T2 signal with internal susceptibility artefact on the haemosiderin staining that are consistent with a haemorrhagic lesion. Longstanding poorly defined subcortical hyperintense lesion in the left superior posterior frontal lobe is lateral to the new haemorrhagic lesion.
The cerebellar lesion is stable.
IMPRESSION: New large left frontal mass with evidence of internal haemorrhage has atypical characteristics for demyelinating disease and is associated with localised mass-effect. Apart from atypical tumefactive plaque, the main diagnostic consideration would be malignancy.
The patient was recalled to a full MRI examination with tumour protocol.
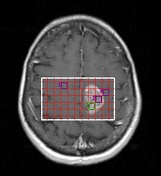

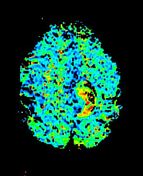
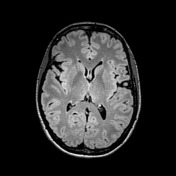
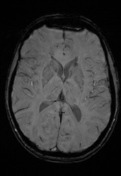
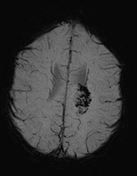
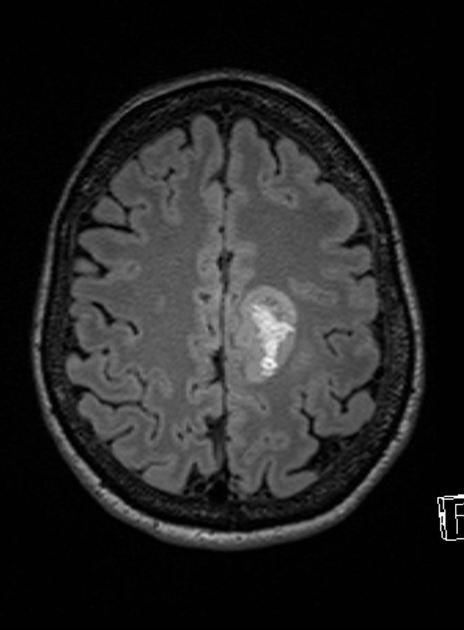
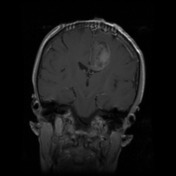
Reference is made to the previous MRI scan. The expansile lesion predominantly in white matter of the left superior frontal and the left cingulate gyri with inferior extension in the left side of the posterior body of the corpus callosum demonstrates T1 and T2 hyperintense haemorrhagic changes laterally and inferiorly. Postcontrast images reveals enhancement in the periphery of the lesion and in the solid T1 hypointense and T2 mildly hyperintense superomedial component of the mass. The non-haemorrhagic enhancing superomedial component demonstrates increased relative cerebral blood volume (CBV). There is also increased cerebral blood volume in the periphery of the lesion. MR spectroscopy sampling of the haemorrhagic component demonstrates increase of lactate peak with relative preservation of NAA peak. There is an incomplete halo of flair signal hyperintensity anteriorly in the left centrum semiovale. There is unchanged appearance of the remaining brain parenchyma.
IMPRESSION: There is partly haemorrhagic expansile lesion in left superior frontal and the left cingulate gyri. The differential diagnosis is of tumour versus tumefactive demyelinating plaque with haemorrhage. The presence of high cerebral blood volume (rCBV) in the non-haemorrhagic enhancing superomedial component of the lesion favours tumour rather than demyelination.


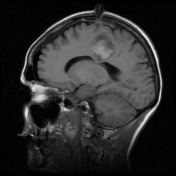

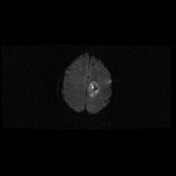




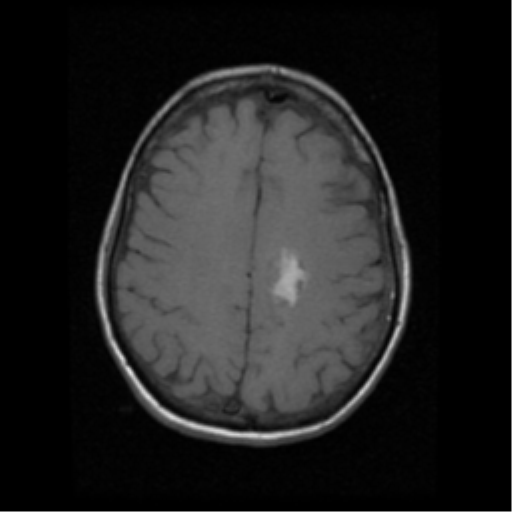
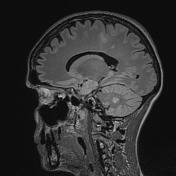
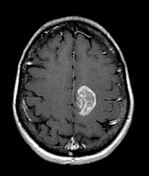
Left parietal mini-craniotomy has been performed, underlying which there is a very small extra-axial collection and dural thickening. Pneumocephalus overlies the anterior left frontal lobe. Expansile mass in the left superior frontal and cingulate gyri extending into the left side of the posterior body of the corpus callosum is again demonstrated (compared with diagnostic MRI performed some days earlier). New focus of intrinsic T1 hyperintensity and FLAIR hypointensity at the superior margin of the mass is in keeping with blood related to the recent biopsy. At this location, the mass demonstrates less solid contrast enhancement consistent with partial tumour excision. The remainder of the lesion is unchanged in appearance, demonstrating central and peripheral contrast enhancement and evidence of haemorrhage. A small amount of surrounding FLAIR hyperintensity is stable.
No hydrocephalus. No diffusion restriction to suggest acute infarction. Non-enhancing FLAIR hyperintense lesion in the left middle cerebellar peduncle is unchanged.
IMPRESSION: Post-biopsy appearances in the left frontal mass.
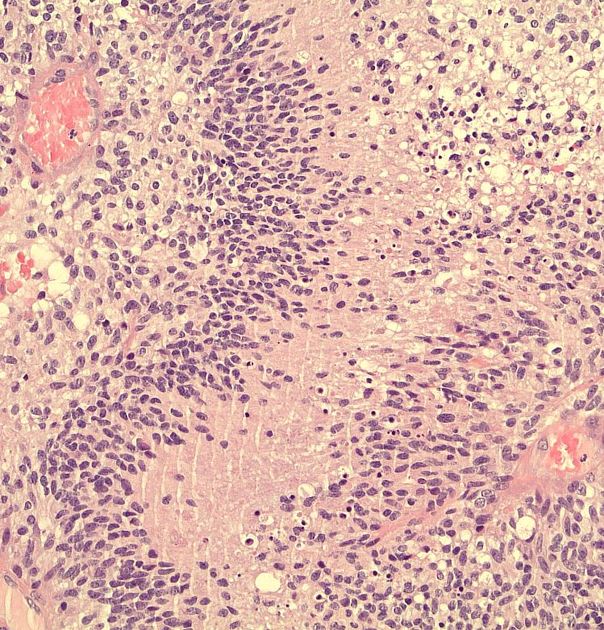
MICROSCOPIC DESCRIPTION: Paraffin sections show fragments of a densely hypercellular astrocytic glioma. Tumour cells have predominantly fibrillary astrocytic morphology and show moderate nuclear and cellular pleomorphism. Scattered mitotic figures are identified. There is prominent microvascular proliferation with multi-layering of atypical cells around vessel lumena. In addition, there are areas of palisaded necrosis incorporating thin-walled necrotic and thrombosed blood vessels. The features are of glioblastoma multiforme (WHO Grade IV). Neither oligodendroglioma or primitive neuroectodermal tumour components are identified.
FINAL DIAGNOSIS: glioblastoma
Note: IDH mutation status is not provided in this case and according to the current (2016) WHO classification of CNS tumours, this tumour would, therefore, be designated as a glioblastoma NOS.
Case Discussion
This cases illustrates a rare presentation of glioblastoma multiforme (GBM) in a patient diagnosed with multiple sclerosis (MS).
There is no well established risk of patients with MS have in developing cancer. There are case reports in the literature describing GBM and primary CNS lymphoma in patients that were followed due MS.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.