Presentation
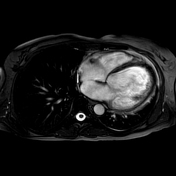
New onset heart failure. Left bundle branch block on ECG. Recent history of Covid 19. Increased CRP and massively increased NT-proBNP. Dilated left ventricle with reduced ejection fraction on TTE, only mild aortic and mitral valve insufficiency. Obstructive CAD was ruled out by coronary angiography.
Patient Data





















Heart rate: 58 bpm, hematocrit: 0.45
Image quality: mild respiratory artifacts, otherwise no limitations
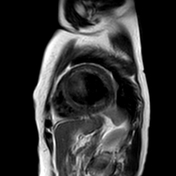
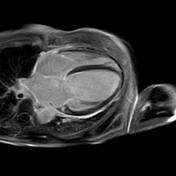
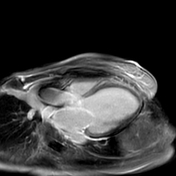
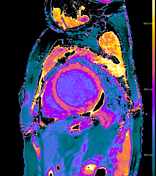
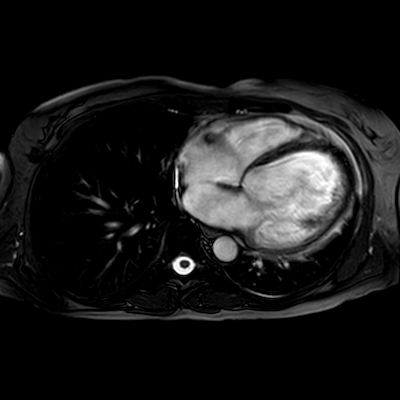
Morphology and functional analysis (endo-volume):
LV-EDVI: 200 mL/m²
LV-ESVI: 147 mL/m²
LV-SVI: 53 mL/m²
LV-EF: 27%
cardiac output: 4.7 L/min
cardiac index: 3.1 L/min/m²
LV-ED wall mas index (without papillary muscles): 87 g/cm²
septum thickness: 8 mm
Diffuse global hypokinesia.
Visually normal atrial size.
Minimal mitral valvular insufficiency.
No intracavitary thrombi.
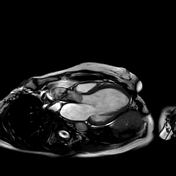
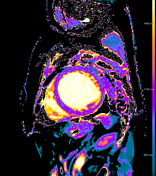
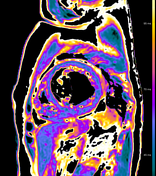
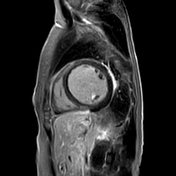
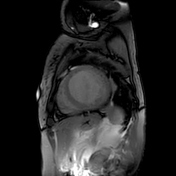
Myocardial tissue properties
questionably minimal myocardial edema on STIR
T2 mapping: mildly elevated in inferior midventricular and basal segments (z-score ~2)
native T1 mapping: mildly elevated inferiorly, but many artifacts are seen on confidentiality map (black dots)
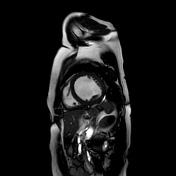
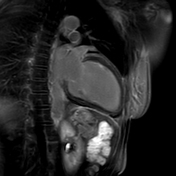
Pericardial late gadolinium enhancement (LGE) best visible in the basal and midventricular anterolateral and inferolateral free walls, minimal pericardial effusion.
Minimal left pleural effusion.
Impression:
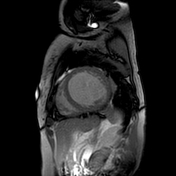
Cardiac MRI findings are consistent with dilated cardiomyopathy and residual inflammatory changes of the pericardium probably as a result of perimyocarditis.
Case Discussion
A case of heart failure with reduced ejection fraction (HFrEF) with severely dilated left ventricle in a fairly young female patient, not sufficiently explained by abnormal loading conditions or coronary artery disease. In the absence of any endocrine or metabolic derangements, autoimmune or infiltrative systemic disease and any toxic or drug-related causes the heart failure was attributed to her recent COVID-19 infection.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.