Presentation
Three-day history of sudden-onset headache, worsening over the past few days. Vomiting, some confusion, and now experiencing double vision with horizontal nystagmus. Previously well.
Patient Data
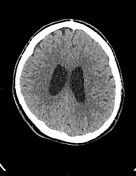




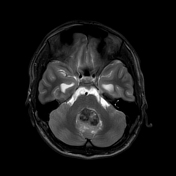
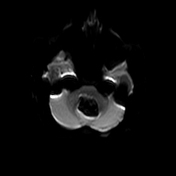
An ovoid mass arises in the midline of the cerebellum, in proximity to the fourth ventricle. Hyperdense is slightly heterogeneous without contrast, possibly with a little calcification.
The fourth ventricle appears effaced, and there is possibly also some mass effect on the cerebral aqueduct. Associated obstructive hydrocephalus, with generalized dilatation of the third and lateral ventricles.
No abnormality was detected in the supratentorial brain parenchyma.
There is an incidental small arachnoid cyst anteriorly in the left temporal fossa.
The extra-axial spaces appear preserved.
Occipital protuberance of the skull is relatively prominent, but is considered within normal limits.
Overall, unremarkable skull appearances.
Conclusion:
Hyperdense posterior fossa mass, highly suspicious for a medulloblastoma, causing obstructive hydrocephalus.

















Head:
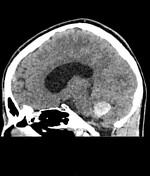
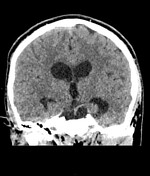
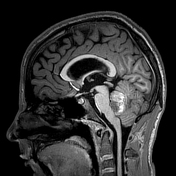
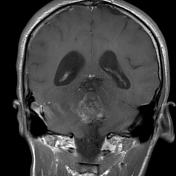
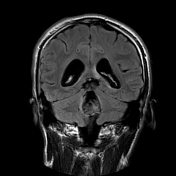
Tip of right frontal EVD centered within the frontal horn of the right lateral ventricle.
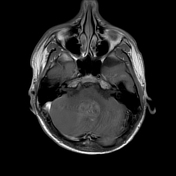
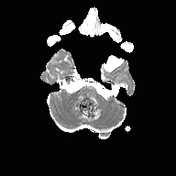
The large heterogenous, lobulated mass which appears to arise from the cerebellar vermis and occupies the fourth ventricle. There is an associated mass effect on both cerebellar hemispheres and the brainstem and subsequent obstructive hydrocephalus of the third and lateral ventricles, the degree of which has improved since EVD insertion.
The mass has a T2 low signal with a surrounding T2 high signal. Heterogeneous T1 high signal is probably a mixture of calcification and hemorrhage. Minor peripheral enhancement. Diffusion-weighted imaging is not useful because of T2 blackout. Low to intermediate signal on FLAIR.
Minor mass effect on the posterior pons and medulla. No tonsillar descent identified. Cerebral aqueduct widely patent consistent with raised intracranial pressure.
Incidental arachnoid cyst anterior to the left temporal lobe (maximum axial measurement 29 mm).
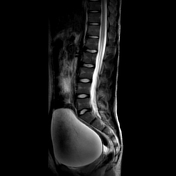
Spine:
The conus terminates at L1 and returns normal signal. No spinal cord mass.
T1 and T2 bright rounded, well-circumscribed lesion within the T9 vertebral body is consistent with a hemangioma. No other vertebral body and disc abnormality.
Mild degenerative change at the L4/L5 disc.
Significantly distended urinary bladder. No clinically significant extra-CNS findings.
Conclusion:
Posterior fossa mass with characteristics consistent with calcification and some hemorrhage.
Minor surrounding edema. The central mass associated with fourth ventricle. Appearances continue to favor medulloblastoma.
The patient went on to have a resection.
Macroscopic features
the specimen consists of several fragments of cream and hemorrhagic tissue with an aggregate measurement of 18 x 14 x 5 mm
the specimen consists of a nodule of brown/hemorrhagic tissue measuring 14 x 10 x 7 mm
Histology
Sections show neural tissue infiltrated by a highly cellular neoplasm composed of intermediate to large-sized cells with rounded, hyperchromatic, pleomorphic nuclei, showing prominent nucleoli, and minimal cytoplasm. Numerous large bizarre, occasionally multinucleate, tumor giant cells are identified, showing striking nuclear pleomorphism, variable rhabdoid morphology, nuclear molding and cell wrapping. No convincing neuroblastic rosettes are identified.
The tumor has a predominantly diffuse sheet-like and vaguely nodular growth pattern with intervening vascular septae. Mitotic figures, including numerous atypical forms, are readily identified. No convincing intrinsic tumor necrosis is identified. Scattered deposits of golden-brown pigment, presumably hemosiderin, are identified, indicative of previous hemorrhage.
Immunohistochemistry
The tumor shows variable expression of GFAP and synaptophysin. There is strong nuclear expression of INI-1. There is no significant expression of NeuN. There is focal nuclear expression of beta-catenin within the smaller cells but only cytoplasmic staining seen in the larger, pleomorphic cells. There is focal expression of desmin in both the conventional round blue cell component and occasional larger cells with apparent rhabdoid morphology. SMA highlights the vessels, although occasional tumor cells also appear positive. There is no significant staining with myogenin. Strong nuclear expression of p53 is noted in occasional tumor cells only. A notable number of tumor cells show membranous expression of CD99, particularly the more pleomorphic component. The MIB1 proliferation index is high.
Molecular markers
CTNNB1 variant identified on NGS is consistent with a WNT-activated medulloblastoma
MYC amplification on FISH has been confirmed
Comment
The histological classification is difficult in this case, as there is a large part of the tumor with a more classic morphology. However, there are significant areas with large cell and anaplastic change. Therefore, we feel on balance this is probably best regarded as a large cell/anaplastic medulloblastoma, WHO grade 4. Occasional cells have a somewhat rhabdomyoblastic appearance and a notable number of cells show strong immunoreactivity for desmin, in keeping with focal myogenin differentiation.
Expert review
The histology has been reviewed with Prof. *****. As mentioned in the initial report, there is considerable large cell /anaplastic change but there are also significant areas that appear classic. Additionally, there are subtle features that suggest divergent differentiation. However, on balance, we agree with the local diagnosis favoring a large cell / anaplastic histological subtype.
Integrated diagnosis
Note: based on WHO 2016 Edition 4e
medulloblastoma - favoring large cell/anaplastic
medulloblastoma WNT-activated
histological grade IV
molecular data: WNT-activated (by immunohistochemistry and methylation analysis), MYC but not MYCN amplification (by FISH), TP53-mutant (by sequencing), CTNNB1-mutant (by sequencing)
Case Discussion
This is an example of a WNT-activated medulloblastoma with associated obstructive hydrocephalus on the initial CT. This the least common subtype of medulloblastoma (approximately 11% of medulloblastomas) but has the best prognosis with long-term survival of almost 100%.
Interestingly, even those with anaplastic histology have a good prognosis, which is not the case with other subgroups.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.