Presentation
Hospital admission 10 days prior due to chest pain, minimal ST-elevation on ECG I+II+AVF, V2-V6, and signs of incomplete left bundle branch block. Negative serial high-sensitive troponins ruled out myocardial infarction. Slightly increased c-reactive protein and leukocytosis.
Patient Data



















Findings:
Heart rate: ~65 bpm, hematocrit: 0.4
Image quality: good, occasional artifact, some movement artifacts on T1 & T2 mapping
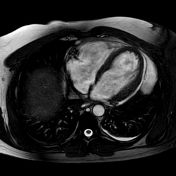
Morphology and functional analysis (endo-volume):
LV-EDVI: 88 mL/m²
LV-ESVI: 40 mL/m²
LV-SVI: 48 mL/m²
LV-EF: 55%
cardiac output: 7.0 L/min
cardiac index: 2.8 L/min/m²
LV-ED wall mass index (without papillary muscle): 62 g/m²
Septum thickness: max. 12 mm
Findings:
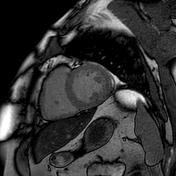
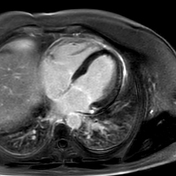
mild global hypokinesia.
no regional left ventricular wall motion abnormalities.
visually normal atrial size
no significant cardiac valve pathology
no intracavitary thrombi
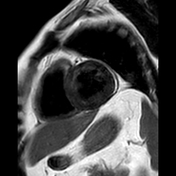
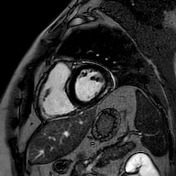
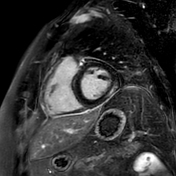
intense pericardial enhancement, mild pericardial effusion on the left free lateral wall
minimal bilateral pleural effusions
Myocardial tissue properties
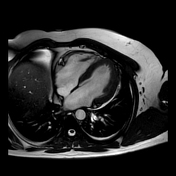
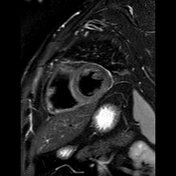
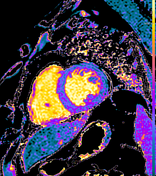
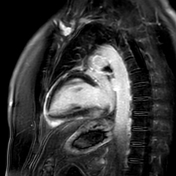
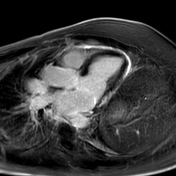
Mildly high signal in the inferoseptal, inferior and inferolateral basal and midventricular segments on the STIR sequence indicating myocardial edema (T2SI ratio >2)
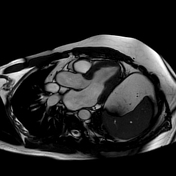
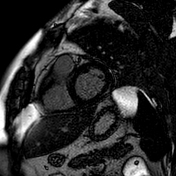
Relatively intense pericardial enhancement as well as subepicardial and patchy intramyocardial late gadolinium enhancement (LGE) visible in the inferolateral and inferior basal segments.
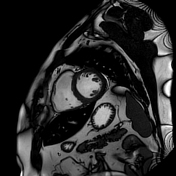
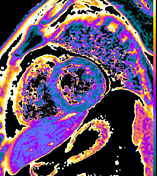
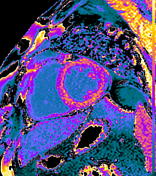
T1 mapping native: mildly increased ~1060-1080 in basal inferoseptal and inferolateral segments
extracellular volume (ECV): mildly increased 32-35% inferolaterlly
T2 mapping: more inhomogeneity and throughout higher values in inferior than anterior segments
*Normal reference ranges based on local data:
native T1: 940-1060 ms; ECV: >32%; T2: 44-56 ms
Impression:
Inflammatory changes of the pericardium and basal inferior and inferolateral myocardium indicate perimyocarditis.
Exam courtesy: Kirsten Fleckstein (radiographer)
Case Discussion
A case of myopericarditis (pericarditis with myocardial involvement) displaying corresponding features on cardiac MRI.
The intense pericardial enhancement and the T1-based Lake Louise criteria suggesting myocardial injury 1 are easily detectable, whereas the recognition of myocardial edema is more difficult here, which also lead to our conclusion that pericarditis is the leading type of inflammation in this case. Calculating the T2 signal intensity ratio between the myocardium and skeletal muscle within the same image and comparing the inferior segments with the remote anterior wall segments for STIR images and T2 mapping helped in the diagnosis of myocardial involvement. The relatively low T2 mapping values might suggest an improvement in the course of the disease 2,3 and support the above thesis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.