Presentation
Rectal malignancy. Concerns of post operative rectovesical fistula.
Patient Data




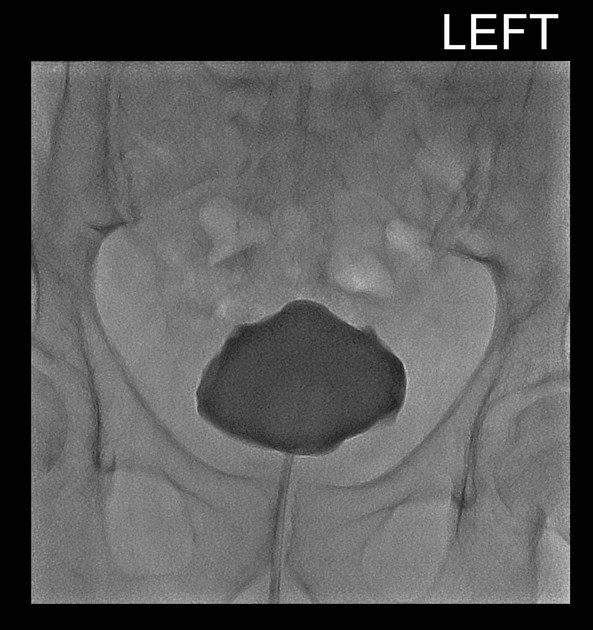
Fistulous tract from the posterior bladder to the upper rectum.
Case Discussion
Classic fluoroscopic appearances of a rectovesical fistula.
Many consider fluoroscopic studies from an era of 'dinosaur radiology'. There are several indications where it remains the 'bees-knees', one being the assessment of fistula and leaks.
It's truly dynamic, unlike a CT with contrast squirted into a tube before any pictures are taken.
Two other practical tips:
- with the bladder always screen initially in the lateral position. Small leaks, the origins of them or fistula may be missed by the covering contrast filled bladder.
- fill the bladder until the patient's toes curl. This ensures the bladder is sufficiently distended and pressurised to ensure a false negative study doesn't occur.
The patient will thank you later for getting it right rather than missing it by not distending the bladder well enough.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.