Presentation
This 49 yo male had a significant knock to the right side of his head. He proceeded to bed, however was noted to be unresponsive and snoring loudly at 4am. An ambulance was called a MRI brain was performed.
Patient Data




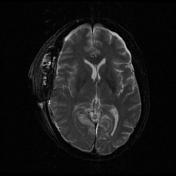

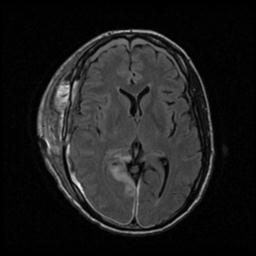
Right posterior cerebral artery infarct, signal abnormality in the left cerebral peduncle and right medial frontal lobe are likely related to subfalcine and descending tentorial herniation at time of presentation.
Acute on chronic right and small chronic left subdural haematomas, with midline shift to the left.
Right globus pallidus infarct.
Case Discussion
Post-traumatic cerebral infarction (PTCI) is a complication of traumatic brain injury with an incidence of 1.9-10.4% of all patients with traumatic brain injury 1. It is associated with a very high mortality rate of 75%.
Aside from the initial traumatic mechanism, patients may also present with neurological signs consistent with the area of infarction.
The most common pattern of PTCI is that of posterior cerebral artery infarction. This has been postulated to be due to compression of the PCA against the the tentorium as the medial temporal lobe herniates caudally 1,2.
Management of PTCI is controversial. Ham et al suggested that aggressive interventional management should be considered in patients with non-malignant (non-MCA region) PTCI, as well as patients with a GCS higher than 5. Patients with malignant PTCI or a GCS lower than 5 invariably do poorly, and Ham et al suggested that intervention would be of little benefit to the patient.
Case contributed by A/Prof. Pramit Phal.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.