Presentation
Bilateral leg sensory changes and saddle anaesthesia. Cauda equina syndrome?
Patient Data
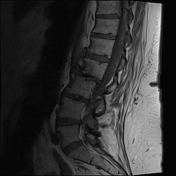




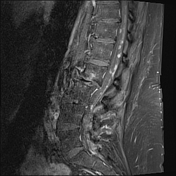


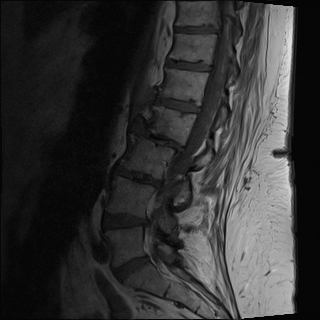
Degenerative discs, particularly at L2-3. Multilevel facet joint arthropathy with synovial enhancement at the left L5-S1 and lesser extent left L4-5 facet joints. Moderate L3-4 spinal canal stenosis.
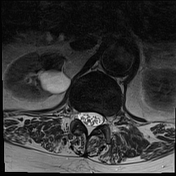
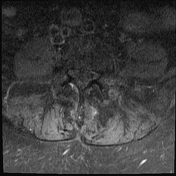
Within the spinal canal, there are innumerable intradural enhancing nodules adjacent and probably adherent to the cauda equina roots. No intramedullary spinal cord mass.
Mild enhancement in the inferior L2 vertebral body, favoured to be degenerative in nature. No suspicious enhancing osseous lesion. Left renal cysts. No paraspinal or retroperitoneal mass.
The patient went on to further imaging including completion neuroaxis MR imaging, which demonstrated a small paraspinal enhancing mass in the upper thoracic spine, potentially in a nerve root dural sheath. No intracranial disease was seen. No widespread disease on CT CAP. A core biopsy was performed of the paraspinal mass.
HISTOPATHOLOGY
MACROSCOPIC: Left mass biopsy – 6 soft fragments of tissue 8 mm in greatest dimension. A fresh specimen has been received and sent for flow cytometry analysis.
MICROSCOPIC: Sections through these fragments of tissue show part of a high grade lymphoid neoplasm. Large atypical lymphoid cells infiltrate as sheets and are seen surrounding and partially destroying bone. The cells have significantly enlarged round or oval nuclei, focally irregular. Some cells have a prominent nucleolus. There are conspicuous apoptotic cells and mitotic figures, as well as areas of necrosis.
Immunohistochemistry has been performed. The neoplastic cells stain positively with CD 45, CD 20, PAX 5, CD 10, BCL2 and BCL6. CD3 stains background T cells. C–MYC is negative (variable, however overall this marker stains no more than 20% of the neoplastic cells). MUM–1 is negative (stains 5% of the neoplastic cells at most). The proliferative index (Ki–67) is approximately 75%. EBER ISH is negative.
FLOW CYTOMETRY: There is a monoclonal B–cell population which is CD 19+ CD20 + CD22 + kappa +, and CD5 – CD10 –.
DIAGNOSIS: These morphological and immunohistochemically features are those of a diffuse large B–cell lymphoma, NOS. There is no evidence of background follicular lymphoma within this specimen.
Case Discussion
Spinal leptomeningeal lymphoma is uncommon. The presumption in this case, is that this is primary spinal leptomeningeal disease given the absence of widespread lymphadenopathy or intracranial disease.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.