Multiple sclerosis
Updates to Article Attributes
Multiple sclerosis (MS) is a relatively common acquired chronic relapsing demyelinating disease involving the central nervous system. It is by definition disseminated not only in space (i.e multiple lesions), but also in time (i.e. lesions are of different age).
A number of clinical variants are recognised, each with specific imaging findings and clinical presentation. They include:
- classic multiple
sclerorissclerosis (Charcot type) - tumefactive multiple sclerosis
- acute malignant Marburg type
- Schilder type (diffuse cerebral sclerosis)
- Balo concentric sclerosis (BCS)
This articles concerns itself primarily with classic (Charcot type) multiple sclerosis. The other variants are discussed separately.
Of note neuromyelitis optica (Devic disease) was considered a variant but is now recognised as a distinct entity.
Epidemiology
Presentation is usually between adolescence and the sixth decade, with a peak at approximately 35 years of age 12. There is a strong, well recognised female predilection with a F:M ratio of 2-3:1.
Multiple sclerosis has a fascinating geographic distribution: it is rarely found in equatorial regions, with incidence gradually increasing with distance from the equator 12.
Clinical presentation
Clinical presentation is both highly variable acutely, as a result of varying plaque location as well as over time, with a number of patterns of longitudinal disease being described 11-12:
-
relapsing–remitting
- most common (70% of cases)
- patients exhibit periodic symptoms with complete recovery (early on)
-
secondary progressive
- approximately 85% of patients with relapsing-remitting MS eventually enter a secondarily progressive phase
-
primary progressive
- uncommon (10% of cases)
- patients do not have remissions, with neurological deterioration being relentless
- progressive with relapses
-
benign multiple sclerosis ~ RIS
(radiologically(radiologically isolated syndrome)- 15-50% of cases
- defined as patients who remain functionally active for over 15 years
As is evident from this list, there is overlap, and in some cases patients can drift from one pattern to another.
Upon presentation patients often have evidence of multiple previous asymptomatic lesions, and the diagnosis of multiple sclerosis can be strongly inferred. In other instances patients present with the first plaque. This is known as clinically isolated syndrome (CIS) and not all patients go on to develop MS.
Symptoms may be sensory or motor or mixed, including cranial nerve involvement, e.g. trigeminal neuralgia or optic neuritis.
Pathology
The exact aetiology is poorly known although it is believed to have both genetic and acquired contributory components. An infectious agent (EBV) or at least catalyst have long been suspected due to the geographic distribution and presence of clusters of cases, however no agent has as yet been firmly identified. Some authors also suggested that "chronic cerebrospinal venous insufficiency" can cause or exacerbate MS but this theory has not been proven by further investigations15.
MS is believed to result from a cellular mediated autoimmune response against ones own myelin components, with loss of oligodendrocytes, with little or no axonal degeneration in acute phase; however, in late stage, loss of oligodendrocytsoligodendrocytes result in axonal degeneration.
Demyelination occurs in discrete foci, termed plaques which range in size from a few millimetres to a few centimeters and are typically perivenular.
Each lesion goes through three pathological stages:
-
early acute stage (active plaques)
- active myelin
break downbreakdown - plaques appear pink and swollen
- active myelin
-
subacute stage
- plaques become paler in colour ("chalky")
- abundant macrophages
-
chronic stage (inactive plaques/gliosis)
- little or no myelin breakdown
- gliosis with associated volume loss
- appear grey/translucent
Patients serum IgG levels tend to be elevated and CSF analysis commonly shows oligoclonal bands.
Associations
- a strong association with HLA-DR2 class II has been identified 11
- Melkersson-Rosenthal syndrome: postulated
Radiographic features
Plaques can occur anywhere in the central nervous system. They are typically ovoid in shape and perivenular in distribution.
CT
CT features are usually non-specific, and significant change may be seen on MRI with an essentially normal CT scan. Features that may be present include:
- plaques can be homogeneously hypo attenuating 8, 11
- brain atrophy may be evident in with long standing chronic MS 5
- some plaques may show contrast enhancement in the active phase 7,11
MRI
MRI has revolutionised the diagnosis and surveillance of patients with MS. Not only can an MRI confirm the diagnosis (see McDonald MRI criteria for multiple sclerosis), but follow-up scans can assess response to treatment and try and determine the disease pattern.
-
T1
- lesions are typically iso- to hypointense (T1 black holes)
- callososeptal interface may have multiple small hypointense lesions (Venus necklace) or the corpus callosum may merely appear thinned 11
-
T2: lesions are typically hyperintense
. -
FLAIR
- lesions are typically hyperintense
- very early sign is called "ependymal dot-dash sign": alternating small foci of hyperintensity along the callososeptal interface 16
- when these propagate centripetally along the medullary venules and arranged perpendicular to lateral ventricles in triangular configuration (extending radially outward -best seen on parasagittal images), they are termed Dawson fingers
- FLAIR is more sensitive than T2 in detection of
juxtracorticaljuxtacortical and periventricular plaques while T2 is more sensitive in infratentorial lesions.
-
T1 C+ (Gd)
- active lesions show enhancement
- enhancement is often incomplete around the periphery (open ring sign)
- DWI/ADC: active plaques may demonstrate restricted diffusion 10-11
- MR spectroscopy: may show reduced NAA peaks within plaques
- double inversion recovery DIR: a new sequence that suppress both CSF and white matter signal and better delineation of the plaques.
Location of the plaques can be infratentorial, deep white matter, periventricular, juxtacortical or mixed white matter-grey matter lesions.
Even on a single scan, some features are helpful in predicting relapsing-remitting vs progressive. progressive disease. Features favouring progressive disease include:
- large numerous plaques
-
hypo intensehypointense T1 lesions
Treatment and prognosis
The aim of treatment is two-foldtwofold: to curtail progression (disease modifying agents) and symptomatic relief.
Steroids, interferon, monoclonal antibodies are all used. Discussion of individual agents is beyond the scope of this article. It is important to remember from an imaging perspective that the use of steroids can make an active lesion reduce in size and reduce enhancement.
Prognosis is variable and depends on the pattern of disease a pattern has (e.g. primary progressive carries a worse prognosis than relapsing-remitting).
In general, patients with relapsing-remitting MS will progress to secondary progressive disease in 10 years, and will require ambulatory aids (e.g. cane/wheelchair/frame) in another 5 to 15 years 12.
Differential diagnosis
The differential diagnosis is dependent on the location and appearance of demyelination. For classic (Charcot type) MS the differential can be divided into intracranial and spinal involvement.
For intracranial disease the differential includes almost all other demyelinating disease as well as:
- CNS fungal infection (e.g. Cryptococcus neoformans) patients tend to be immunocompromised
- mucopolysaccharidosis (e.g. Hurler disease): congenital and occurs in a younger age group
- Marchiafava-bignami disease (for callosal lesions)
- Susac syndrome
- CNS manifestations of primary antiphospholipid syndrome 13
For spinal involvement the following should be considered:
- transverse myelitis
- infection
- spinal cord tumours
, e(e.g. astrocytomas)
The differential for multiple sclerosis variants (e.g. tumefactive MS, Devic disease) are discussed separately.
-<li>classic multiple scleroris (Charcot type)</li>- +<li>classic multiple sclerosis (Charcot type)</li>
-<strong>benign multiple sclerosis ~ RIS (radiologically isolated syndrome)</strong><ul>- +<strong>benign multiple sclerosis ~ RIS (<a href="/articles/radiologically-isolated-syndrome">radiologically isolated syndrome</a>)</strong><ul>
-</ol><p>As is evident from this list, there is overlap, and in some cases patients can drift from one pattern to another. </p><p>Upon presentation patients often have evidence of multiple previous asymptomatic lesions, and the diagnosis of multiple sclerosis can be strongly inferred. In other instances patients present with the first plaque. This is known as <a href="/articles/clinically-isolated-syndrome">clinically isolated syndrome (CIS)</a> and not all patients go on to develop MS. </p><p>Symptoms may be sensory or motor or mixed, including cranial nerve involvement, e.g. <a href="/articles/trigeminal-neuralgia">trigeminal neuralgia</a> or <a href="/articles/optic-neuritis">optic neuritis</a>. </p><h4>Pathology</h4><p>The exact aetiology is poorly known although it is believed to have both genetic and acquired contributory components. An infectious agent (EBV) or at least catalyst have long been suspected due to the geographic distribution and presence of clusters of cases, however no agent has as yet been firmly identified. Some authors also suggested that "chronic cerebrospinal venous insufficiency" can cause or exacerbate MS but this theory has not been proven by further investigations<sup>15</sup> .</p><p>MS is believed to result from a cellular mediated autoimmune response against ones own myelin components, with loss of oligodendrocytes, with little or no axonal degeneration in acute phase; however, in late stage, loss of oligodendrocyts result in axonal degeneration. </p><p>Demyelination occurs in discrete foci, termed plaques which range in size from a few millimetres to a few centimeters and are typically perivenular.</p><p>Each lesion goes through three pathological stages:</p><ul>- +</ol><p>As is evident from this list, there is overlap, and in some cases patients can drift from one pattern to another. </p><p>Upon presentation patients often have evidence of multiple previous asymptomatic lesions, and the diagnosis of multiple sclerosis can be strongly inferred. In other instances patients present with the first plaque. This is known as <a href="/articles/clinically-isolated-syndrome">clinically isolated syndrome (CIS)</a> and not all patients go on to develop MS. </p><p>Symptoms may be sensory or motor or mixed, including cranial nerve involvement, e.g. <a href="/articles/trigeminal-neuralgia">trigeminal neuralgia</a> or <a href="/articles/optic-neuritis">optic neuritis</a>. </p><h4>Pathology</h4><p>The exact aetiology is poorly known although it is believed to have both genetic and acquired contributory components. An infectious agent (EBV) or at least catalyst have long been suspected due to the geographic distribution and presence of clusters of cases, however no agent has as yet been firmly identified. Some authors also suggested that "chronic cerebrospinal venous insufficiency" can cause or exacerbate MS but this theory has not been proven by further investigations <sup>15</sup>.</p><p>MS is believed to result from a cellular mediated autoimmune response against ones own myelin components, with loss of oligodendrocytes, with little or no axonal degeneration in acute phase; however, in late stage, loss of oligodendrocytes result in axonal degeneration. </p><p>Demyelination occurs in discrete foci, termed plaques which range in size from a few millimetres to a few centimeters and are typically perivenular.</p><p>Each lesion goes through three pathological stages:</p><ul>
-<li>active myelin break down </li>- +<li>active myelin breakdown </li>
-</ul><p>Patients serum IgG levels tend to be elevated and CSF analysis commonly shows oligoclonal bands </p><h5>Associations</h5><ul>- +</ul><p>Patients serum IgG levels tend to be elevated and CSF analysis commonly shows oligoclonal bands.</p><h5>Associations</h5><ul>
-<li>lesions are typically iso- to hypointense (<a title="T1 black holes" href="/articles/t1-black-holes-1">T1 black holes</a>) </li>- +<li>lesions are typically iso- to hypointense (<a href="/articles/t1-black-holes-1">T1 black holes</a>) </li>
-<strong>T2:</strong> lesions are typically hyperintense.</li>- +<strong>T2:</strong> lesions are typically hyperintense</li>
-<li>very early sign is called "<a title="ependymal dot-dash sign" href="/articles/ependymal-dot-dash-sign">ependymal dot-dash sign</a>": alternating small foci of hyperintensity along the callososeptal interface <sup>16</sup>- +<li>very early sign is called "<a href="/articles/ependymal-dot-dash-sign">ependymal dot-dash sign</a>": alternating small foci of hyperintensity along the callososeptal interface <sup>16</sup>
-<li>FLAIR is more sensitive than T2 in detection of juxtracortical and periventricular plaques while T2 is more sensitive in infratentorial lesions.</li>- +<li>FLAIR is more sensitive than T2 in detection of juxtacortical and periventricular plaques while T2 is more sensitive in infratentorial lesions</li>
-<strong>double inversion recovery DIR: </strong>a new sequence that suppress both CSF and white matter signal and better delineation of the plaques.</li>-</ul><p>Location of the plaques can be infratentorial, deep white matter, periventricular, juxtacortical or mixed white matter-grey matter lesions.</p><p>Even on a single scan, some features are helpful in predicting relapsing-remitting vs progressive disease. Features favouring progressive disease include:</p><ul>- +<strong><a href="/articles/double-inversion-recovery-sequence">double inversion recovery DIR</a>: </strong>a new sequence that suppress both CSF and white matter signal and better delineation of the plaques.</li>
- +</ul><p>Location of the plaques can be infratentorial, deep white matter, periventricular, juxtacortical or mixed white matter-grey matter lesions.</p><p>Even on a single scan, some features are helpful in predicting relapsing-remitting vs. progressive disease. Features favouring progressive disease include:</p><ul>
-<li>hypo intense T1 lesions</li>-</ul><h4>Treatment and prognosis</h4><p>The aim of treatment is two-fold: to curtail progression (disease modifying agents) and symptomatic relief. </p><p>Steroids, interferon, monoclonal antibodies are all used. Discussion of individual agents is beyond the scope of this article. It is important to remember from an imaging perspective that the use of steroids can make an active lesion reduce in size and reduce enhancement.</p><p>Prognosis is variable and depends on the pattern of disease a pattern has (e.g. primary progressive carries a worse prognosis than relapsing-remitting). </p><p>In general, patients with relapsing-remitting MS will progress to secondary progressive disease in 10 years, and will require ambulatory aids (e.g. cane/wheelchair/frame) in another 5 to 15 years <sup>12</sup>. </p><h4>Differential diagnosis</h4><p>The differential diagnosis is dependent on the location and appearance of demyelination. For classic (Charcot type) MS the differential can be divided into intracranial and spinal involvement. </p><p>For intracranial disease the differential includes almost all other <a href="/articles/demyelination">demyelinating disease</a> as well as:</p><ul>-<li>CNS fungal infection (e.g. Cryptococcus neoformans ) patients tend to be immunocompromised</li>- +<li>hypointense T1 lesions</li>
- +</ul><h4>Treatment and prognosis</h4><p>The aim of treatment is twofold: to curtail progression (disease modifying agents) and symptomatic relief. </p><p>Steroids, interferon, monoclonal antibodies are all used. Discussion of individual agents is beyond the scope of this article. It is important to remember from an imaging perspective that the use of steroids can make an active lesion reduce in size and reduce enhancement.</p><p>Prognosis is variable and depends on the pattern of disease a pattern has (e.g. primary progressive carries a worse prognosis than relapsing-remitting). </p><p>In general, patients with relapsing-remitting MS will progress to secondary progressive disease in 10 years, and will require ambulatory aids (e.g. cane/wheelchair/frame) in another 5 to 15 years <sup>12</sup>. </p><h4>Differential diagnosis</h4><p>The differential diagnosis is dependent on the location and appearance of demyelination. For classic (Charcot type) MS the differential can be divided into intracranial and spinal involvement. </p><p>For intracranial disease the differential includes almost all other <a href="/articles/demyelination">demyelinating disease</a> as well as:</p><ul>
- +<li>CNS fungal infection (e.g. <em>Cryptococcus neoformans</em>) patients tend to be immunocompromised</li>
-<a href="/articles/mucopolysaccharidoses-2">mucopolysaccharidosis</a> (e.g. Hurler disease): congenital and occurs in a younger age group</li>- +<a href="/articles/mucopolysaccharidoses-2">mucopolysaccharidosis</a> (e.g. <a href="/articles/hurler-syndrome">Hurler disease</a>): congenital and occurs in a younger age group</li>
-<li>CNS manifestations of primary antiphospholipid syndrome <sup>13</sup>- +<li>CNS manifestations of primary <a href="/articles/antiphospholipid-syndrome">antiphospholipid syndrome</a> <sup>13</sup>
-<li>spinal cord tumours, e.g. astrocytomas</li>- +<li>spinal cord tumours (e.g. <a href="/articles/spinal-astrocytoma">astrocytomas</a>)</li>
Image ( destroy )
Image ( update )
Image ( update )
Image ( destroy )
Image ( update )
Image ( update )
Image ( update )
Image ( destroy )
Image ( update )
Image ( update )
Image ( update )
Image ( update )
Image ( update )
Image 1 MRI (FLAIR) ( update )

Image 2 MRI (FLAIR) ( update )

Image 3 MRI (T2) ( update )

Image 4 MRI (Axial) ( update )
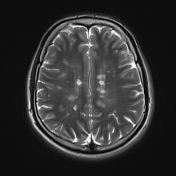
Image 5 MRI (T2) ( update )

Image 6 MRI (T1) ( update )
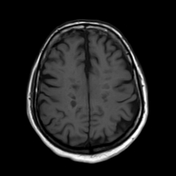
Image 7 MRI (T2) ( update )

Image 8 Annotated image ( create )

Image 9 MRI (T1 C+) ( update )

Image 10 MRI (DIR) ( update )

Image 11 MRI (FLAIR) ( update )

Image 15 MRI (T2) ( update )

Image 16 MRI (T2) ( update )

Image 17 MRI (FLAIR) ( update )

Image 18 MRI (FLAIR) ( update )

Image 19 MRI (T1 C+) ( update )

Image 20 MRI (FLAIR) ( update )

Image 22 MRI (FLAIR) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.