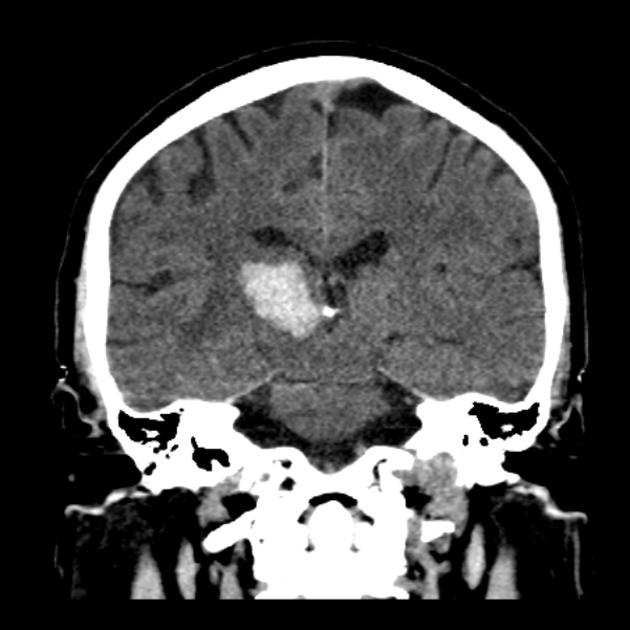
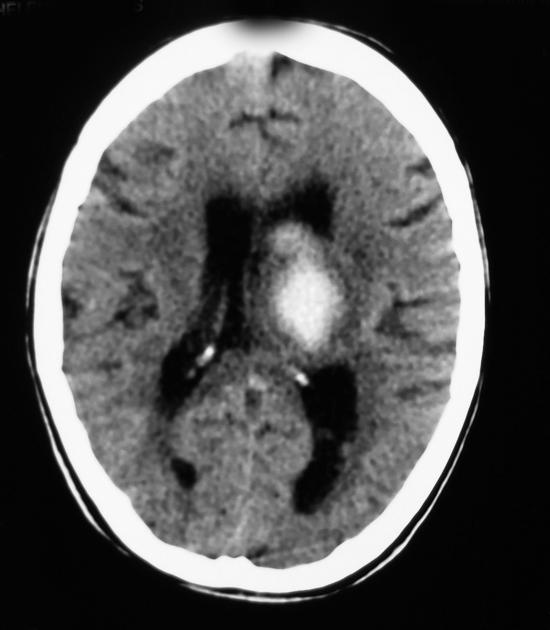
Thalamic hemorrhages are a common form of intracerebral hemorrhage, and usually are a result of poorly controlled long-standing hypertension, although also have other causes. When due to chronic hypertension, the stigmata of chronic hypertensive encephalopathy are often present (see cerebral microhemorrhages).
On this page:
Clinical presentation
The clinical presentation can be incredibly varied, given the thalamus has a central and pivotal role in multiple neural pathways. Potential clinical manifestations may include 2:
downward gaze (paralysis of upward gaze)
small pupils (lack of light pupillary response)
depressed consciousness
apathy
hypersomnolence
disorientation
visual hallucinations
aphasia
neglect
memory deficits
visuospatial dysfunction
pain and sensory anomalies (including Déjerine-Roussy syndrome)
Radiographic features
CT
Thalamic hemorrhage is easily recognisable on CT as hyperdensity within the thalamus.
There are many predictors of hematoma expansion potentially evident on CT, which are discussed in depth in the main intracerebral hemorrhage article.
MRI
The appearance of hemorrhage on MRI varies with time and to some degree the size of the hematoma (see aging blood on MRI).
Treatment and prognosis
Management is generally medical, and does not differ for other causes of intracerebral hemorrhage - please see the article on intracerebral hemorrhage for further discussion 4. In selected patients, there may be a role for decompressive craniectomy 5.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.