Acute cerebellitis and acute cerebellar ataxia represent a spectrum of inflammatory processes characterised by sudden onset cerebellar dysfunction. It usually affects children and is related as a consequence of primary or secondary infection, or much less commonly as a result of a post-vaccination reaction.
On this page:
Terminology
The terms acute cerebellitis and acute cerebellar ataxia are sometimes used interchangeably, as in this article, but they are considered separate by some authors 9. Acute cerebellar ataxia is a clinical diagnosis that can be made without imaging evidence of cerebellar inflammation. Acute cerebellitis may be considered a less common and more severe form of acute cerebellar ataxia 9,10.
Epidemiology
Usually occurring in children under six years of age, acute cerebellar ataxia and acute cerebellitis represent the most common cause of acute ataxia in the paediatric population. It is reported as a complication of several systemic infectious diseases, such as varicella infection (chickenpox) 6.
Adult cases of cerebellitis are possible 5.
Clinical presentation
A broad range of signs and symptoms may be present: fever, appendicular ataxia, truncal ataxia, dysarthria, cerebellar mutism, tremor, nystagmus, headache, nausea, vomiting, and consciousness alterations 11,12. Signs of meningeal irritation and seizures may be observed less frequently 1,4.
Some relevant complications have been described, such as:
obstructive hydrocephalus and consequent intracranial hypertension
cerebellar trunk compression
severe cerebellar atrophy 3
Laboratory findings
CSF pleocytosis 4
Pathology
Acute cerebellitis has been associated with a large number of infectious agents, such as: coxsackievirus, echovirus, enteroviruses, Epstein-Barr virus, hepatitis A, herpes simplex virus 1, human herpesvirus 6, measles, rubella, mumps, parvovirus B19, influenza, rotavirus, Borrelia burgdorferi (Lyme disease), malaria, Mycoplasma pneumoniae, and typhoid fever 2,4,6,11,12.
Acute cerebellar ataxia following vaccination for varicella, hepatitis B, and rabies has been reported 6-8.
Radiographic features
CT
Cerebellar images can be normal due to the limitations of CT in evaluation of the posterior fossa. Nonetheless, complications like compression of the brainstem and obstructive hydrocephalus, when present, are identified on CT images and may guide further investigation.
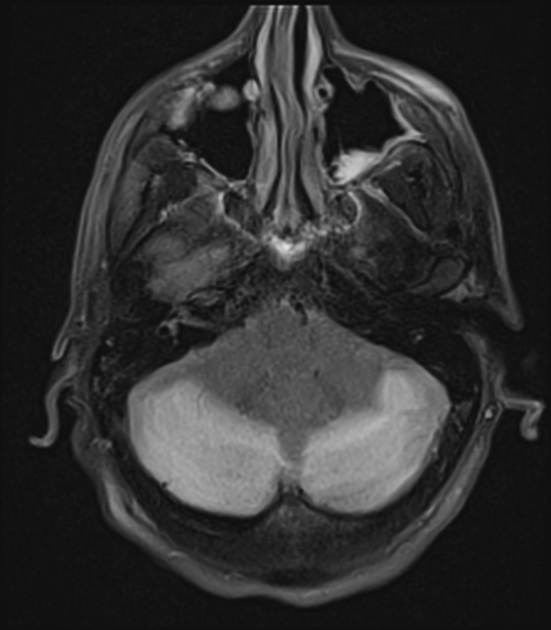
MRI
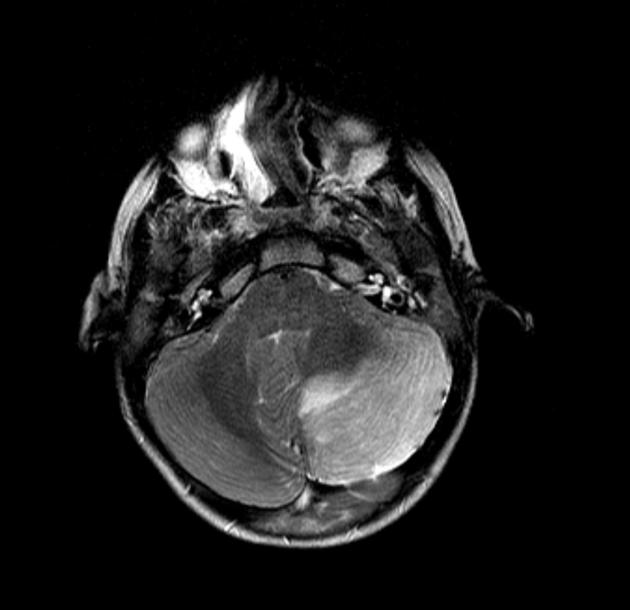
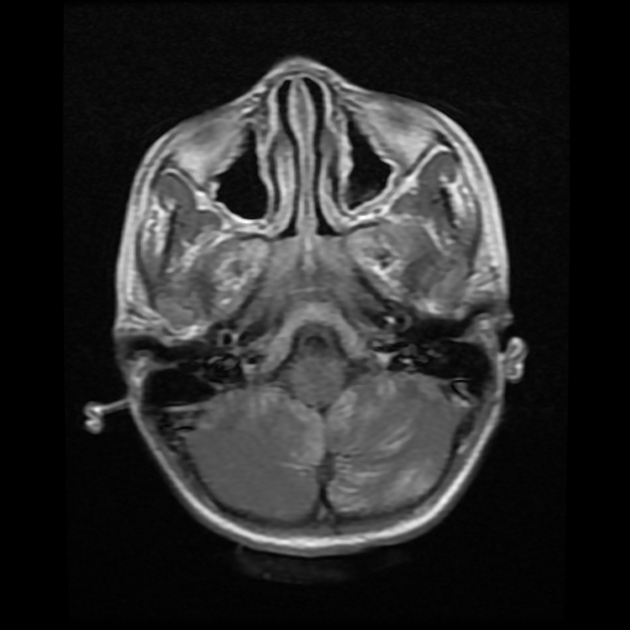
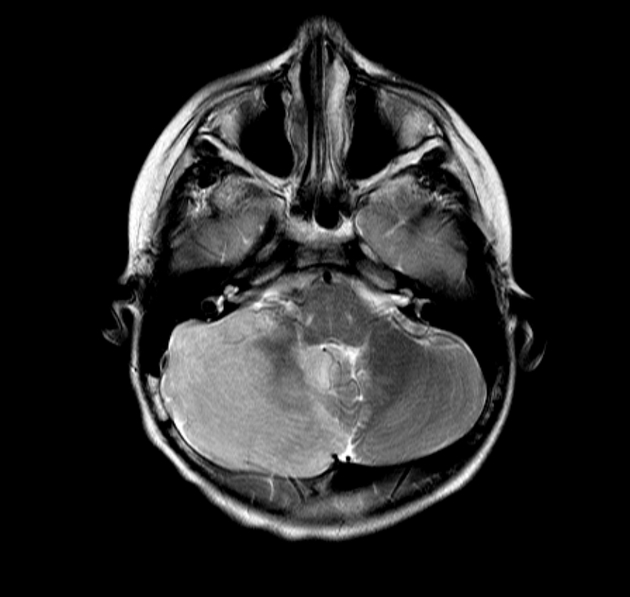
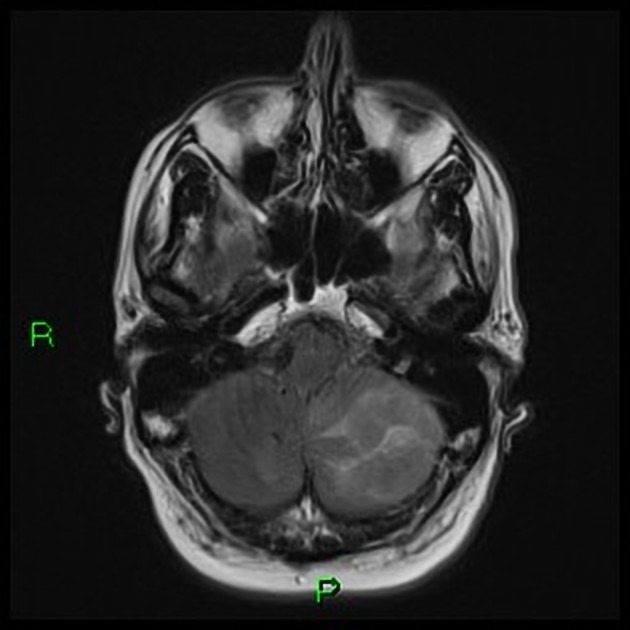
Usually, the cerebellar hemispheres are symmetrically affected, but changes can be unilateral. There be homogeneous mass effect due the cerebellar swelling 1,4. The middle cerebellar peduncles and corpus callosum (see cytotoxic lesions of the corpus callosum) can also be affected 11.
T1: cortical hypointensity
T2/FLAIR: cortical hyperintensity
DWI/ADC: may show restriction due to cytotoxic oedema caused by the acute inflammatory lesions 4
T1 C+ (Gd): cortical and adjacent leptomeninges may show enhancement
Following clinical recovery, cerebellar atrophy may develop 5,13.
Treatment and prognosis
The disease is generally benign and self-limited, however some complications, as described above, can take the patient to a worse prognosis and lead to death.
In rare complicated cases, massive cerebellar oedema can require surgical decompression of the posterior cranial fossa 4.
Differential diagnosis
Clinical features and the age group are essential when thinking of possible differential diagnoses. Acute cerebellitis limited to one cerebellar hemisphere may mimic a cerebellar tumour, especially:
medulloblastoma: atypical cerebellar location usually seen in adult patients
cerebellar lymphoma: elderly patients
Other differentials to consider are:










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.