Acute cholecystitis refers to the acute inflammation of the gallbladder. It is the primary complication of cholelithiasis and the most common cause of acute pain in the right upper quadrant (RUQ).
On this page:
Epidemiology
Acute cholecystitis is a common cause of hospital admission and is responsible for approximately 3-10% of all patients with abdominal pain. Cholelithiasis is the major risk factor and causes up to 95% of cases 14. Other risk factors include AIDS, fibrate (hypolipidemic agent) and ascariasis.
Clinical presentation
Constant right upper quadrant pain that can radiate to the right shoulder. Pain typically persists for more than six hours, in contradistinction to the intermittent right upper quadrant pain of biliary colic. Nausea, vomiting, and fever are also often reported.
Pathology
90-95% of cases are due to gallstones (i.e. acute calculous cholecystitis) with the remainder being acute acalculous cholecystitis.
The development of acute calculous cholecystitis follows a sequence of events:
gallstone obstruction of the gallbladder neck or cystic duct
inflammation from chemical injury of the mucosa by bile salts
reactive production of mucus, leading to increased intraluminal pressure and distention
increased luminal distention restricting blood flow to the gallbladder wall (gallbladder hydrops)
increasing wall thickness from edema and inflammatory changes
secondary bacterial infection in ~66% of patients
Radiographic features
Ultrasound (US) is the preferred initial modality in the investigation of right upper quadrant pain. It is more sensitive than HIDA scintigraphy 4 and more readily available.
Ultrasound
The most sensitive US finding in acute cholecystitis is the presence of cholelithiasis in combination with the sonographic Murphy sign. Both gallbladder wall thickening (>3 mm) and pericholecystic fluid are secondary findings.
Other less specific findings include gallbladder distension and sludge.
Every effort should be made to demonstrate the obstructing stone in the gallbladder neck or cystic duct.
Nuclear medicine
99mTc-HIDA scintigraphy
HIDA cholescintigraphy in acute cholecystitis will demonstrate non-visualization of the gallbladder 4 hours after injection.
Cholescintigraphy is unable to demonstrate many complications of cholecystitis, nor the alternative diagnoses which may be found with ultrasound. It is therefore reserved for the evaluation of sonographically equivocal cases.
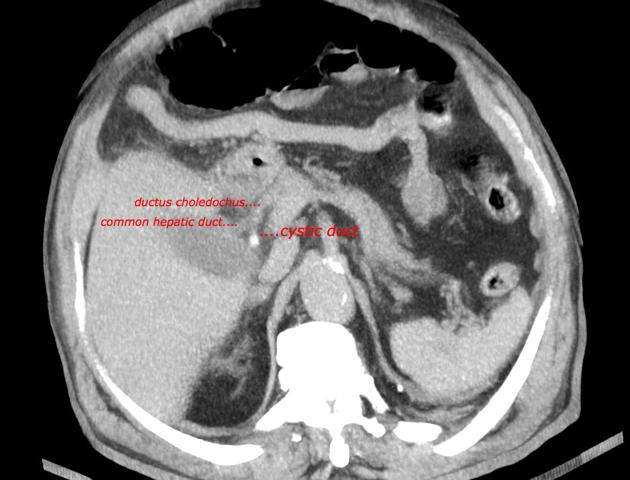
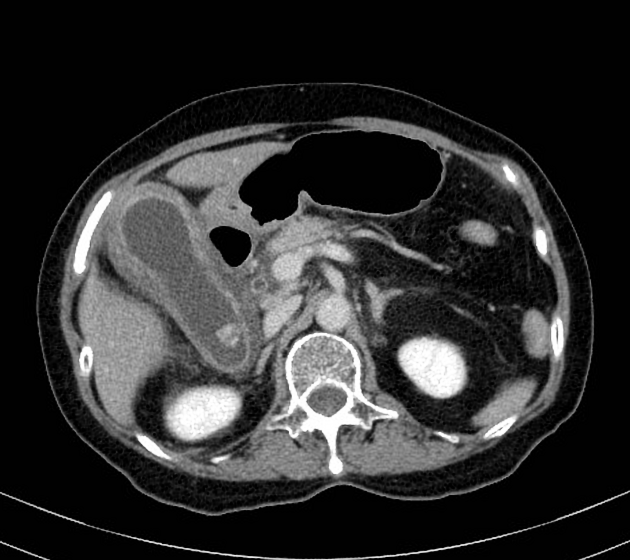
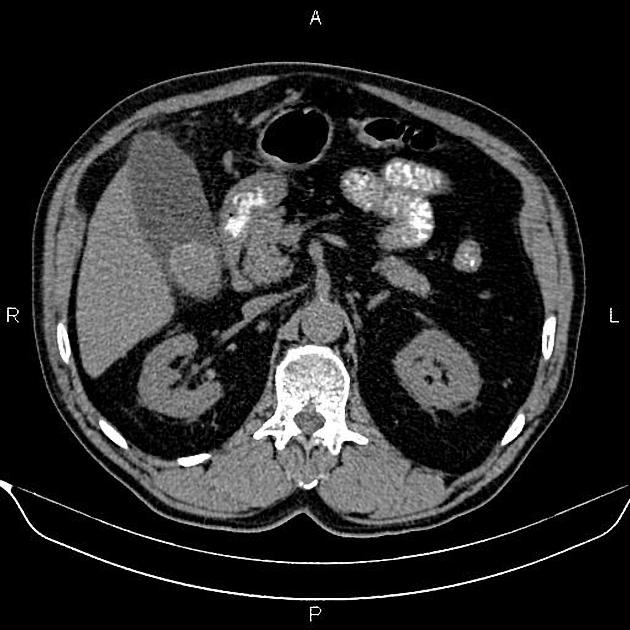
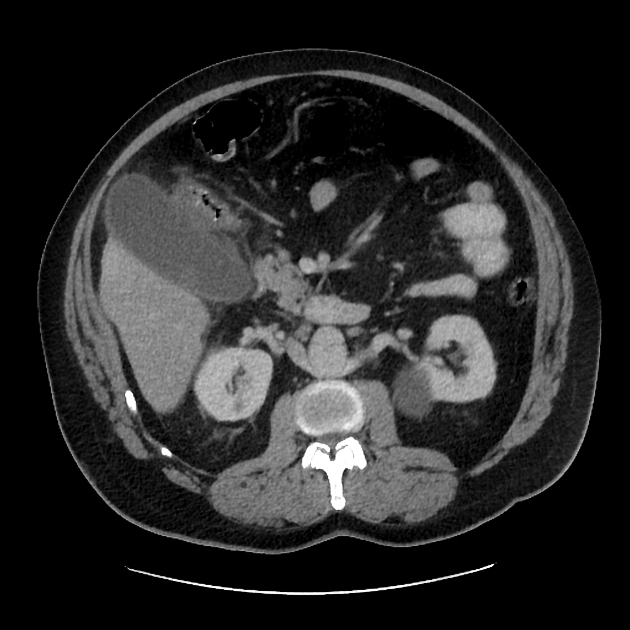
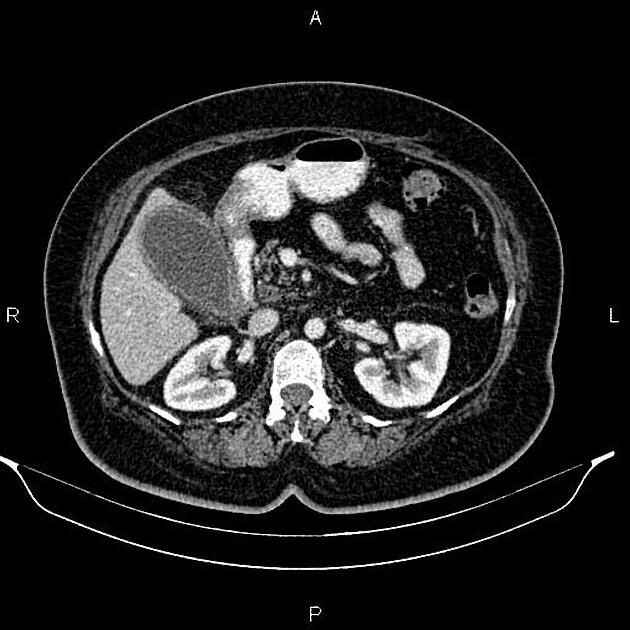
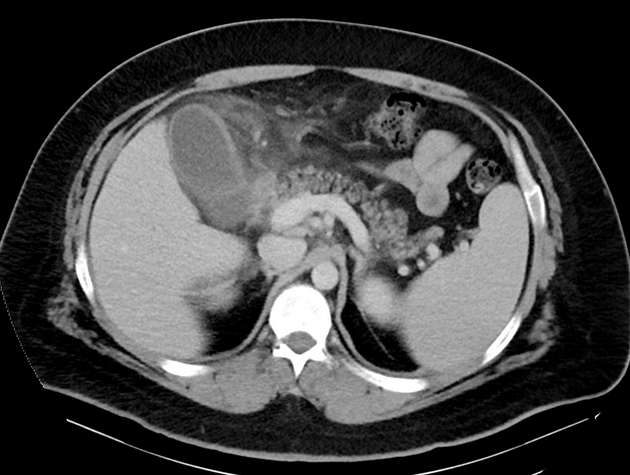
CT
Although traditionally considered less sensitive than ultrasound, some reviews find CT more sensitive for this diagnosis 12,13,15,17. An advantage is that CT also allows better evaluation of other pathologies at the same time. CT findings include 3:
cholelithiasis: gallstones isodense to bile will be missed on CT
gallbladder distension
mural or mucosal hyperenhancement
pericholecystic fluid and inflammatory fat stranding
high-density bile 15
enhancement of the adjacent liver parenchyma due to reactive hyperemia
-
tensile gallbladder fundus sign 7
fundus bulging into and distorting the anterior abdominal wall
~75% sensitivity and ~95% specificity for acute cholecystitis in the absence of any other CT features
useful sign in making an early diagnosis
Diagnostic criteria on CT as proposed by Mirvis et al. include 6:
-
major criteria
gallstones
thickened gallbladder wall
pericholecystic fluid collections
subserosal edema
-
minor criteria
gallbladder distention
sludge
diagnosis of acute cholecystitis can be supported if one major and two minor criteria are present refs
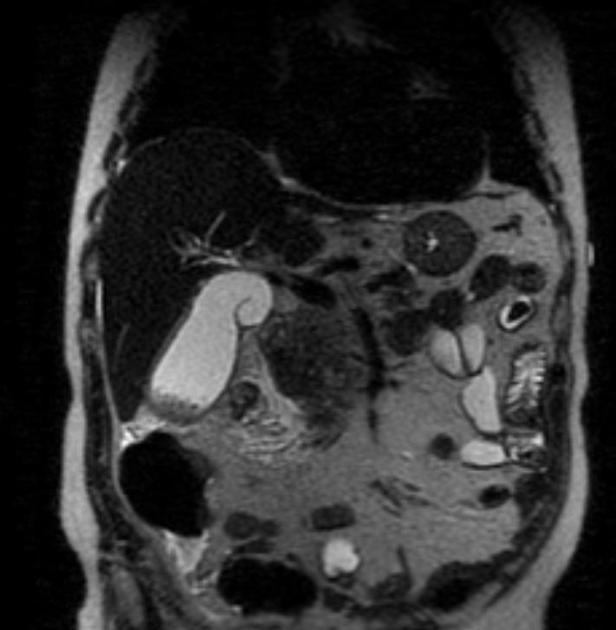
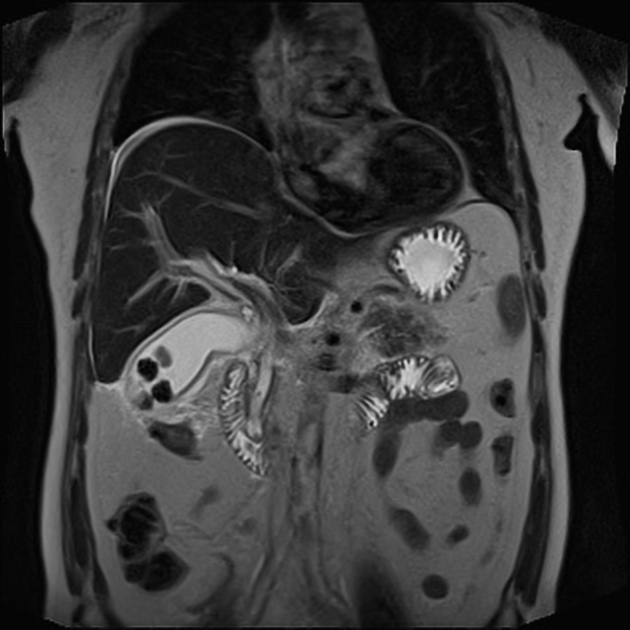
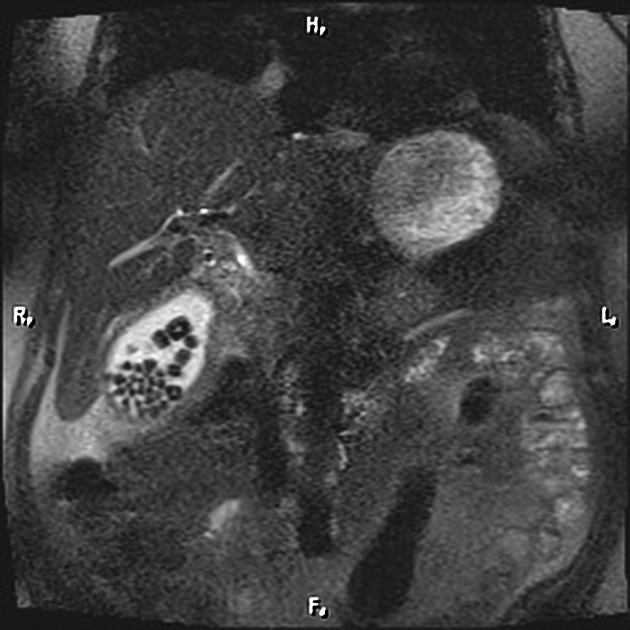
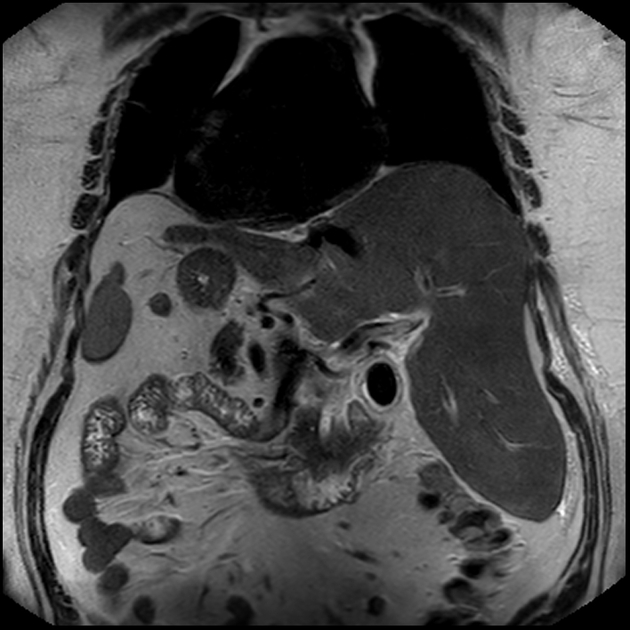
MRI
MRI is sensitive in the detection of acute cholecystitis, with findings similar to those seen on ultrasound and CT 3. MR cholangiopancreatography (MRCP) may show an impacted stone in the gallbladder neck or cystic duct as a rounded filling defect.
Treatment and prognosis
Urgent surgical removal of the gallbladder is the treatment of choice for the uncomplicated disease. Gallbladder ischemia with transmural necrosis may occur if the obstruction persists.
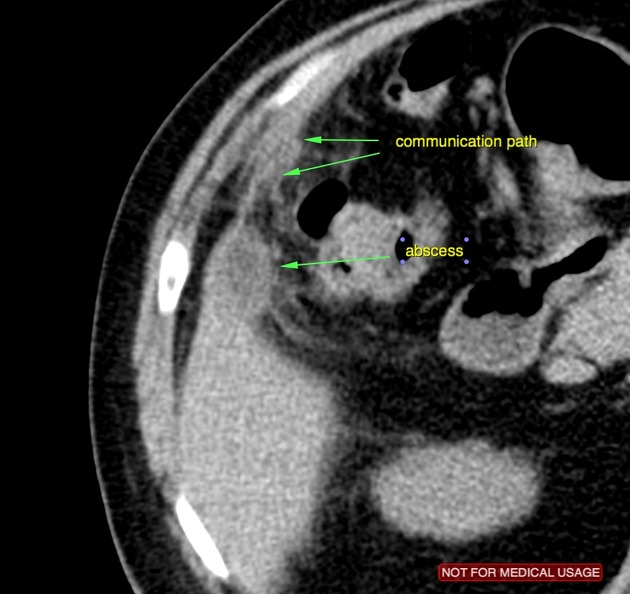
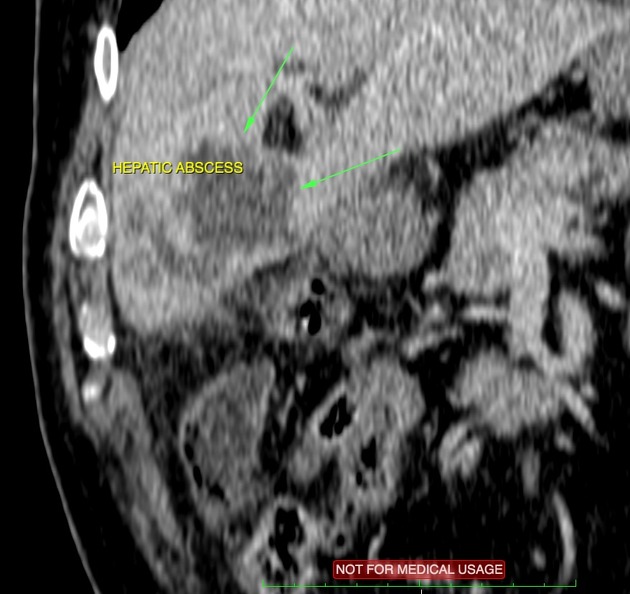
Complications
gangrenous cholecystitis (most common - 20%) 8
gallbladder empyema (5-15%) 18
gallbladder perforation (~5%) 8,9
vascular complications (gallbladder hemorrhage, portal vein thrombosis, cystic artery pseudoaneurysm) 11
Differential diagnosis
The differential diagnosis for acute cholecystitis is extensive and includes:
For a more extensive differential, please refer to the article on the differential diagnosis of diffuse gallbladder wall thickening.