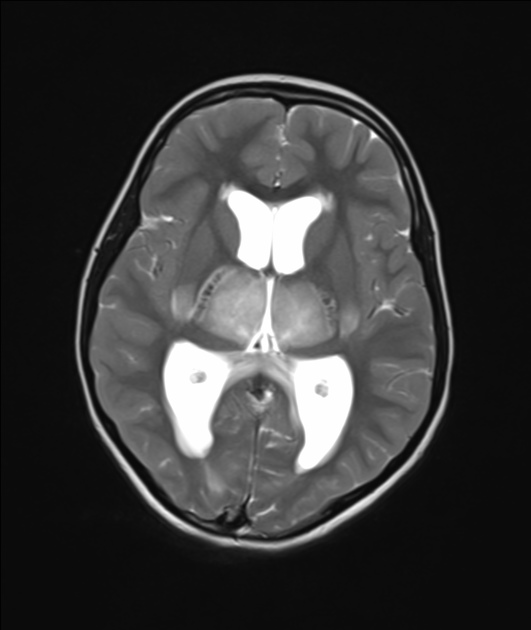
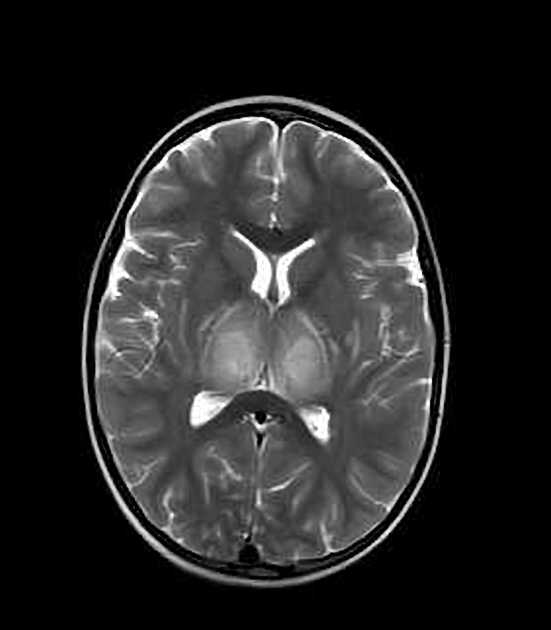
Acute necrotising encephalopathy, also referred as acute necrotising encephalopathy of childhood (ANEC), is a rare type of encephalopathy characterised by multiple bilateral brain lesions, mainly involving the thalami, but also the putamina, internal and external capsules, cerebellar white matter, and the brainstem tegmentum.
On this page:
Epidemiology
Acute necrotising encephalitis is a rare condition. From the first case described in 1995, many cases have been reported in Asia as well as in many Western countries. Most cases are sporadic; however, a few cases of recurrent and/or familial episodes have been reported, secondary to mutations in the RANBP2 gene 10.
Although the initial publications were in the paediatric population, multiple further reports showed the condition to also occur in adulthood 8.
Clinical presentation
Clinically, it is characterised by acute encephalopathy, with dramatic neurological deficits/symptoms. A viral aetiology has been proposed in some cases; viral prodrome may therefore precede the neurological deficits.
Pathology
The aetiology and the pathogenesis of acute necrotising encephalitis are only partially clear. Usually, it develops secondary to viral infections, including influenza A and influenza B, parainfluenza, varicella, enterovirus, and SARS-CoV-2 9.
Pathologically, the lesions show oedema, haemorrhage and necrosis. Acute necrotising encephalopathy is characterised by the lack of inflammatory cells in affected brain parenchyma in comparison to the more common entities of acute disseminated encephalomyelitis and acute haemorrhagic encephalitis 1.
Radiographic features
CT
On CT, the corresponding thalamic, putamina, cerebral, cerebellar and brainstem abnormalities are hypodense.
Intracranial haemorrhage and cavitation may also be seen, both of which are associated with a worse prognosis.
MRI
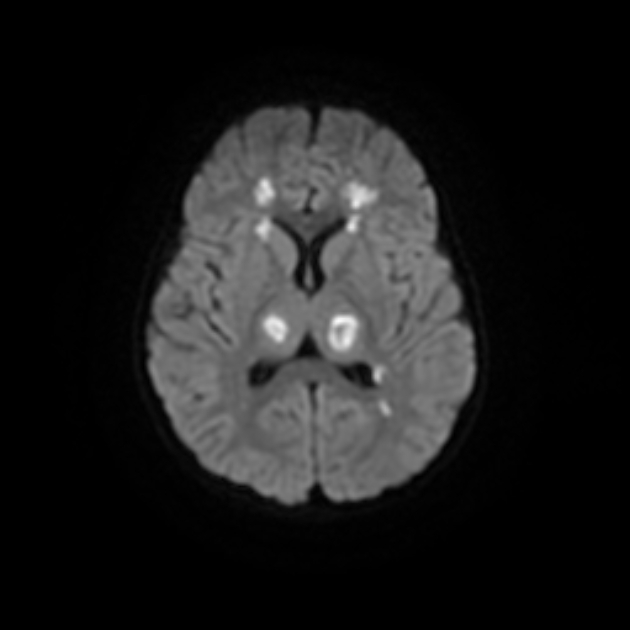
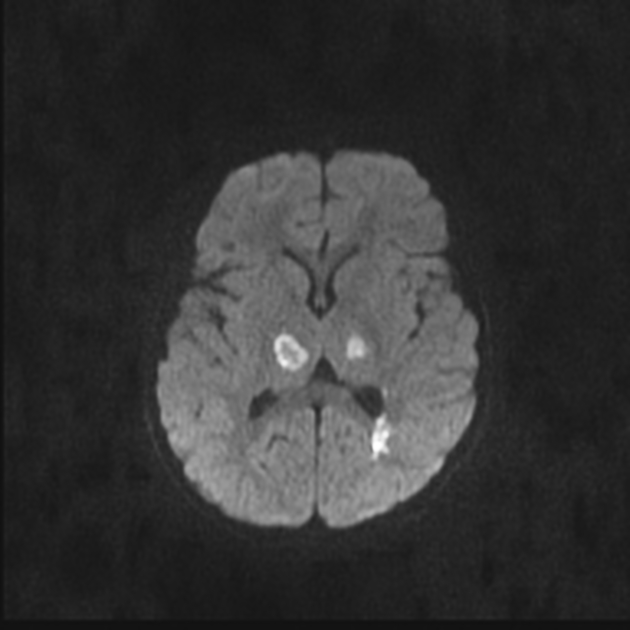
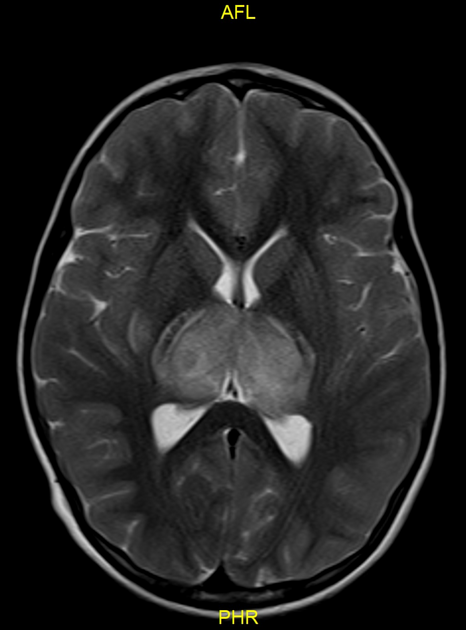
In most cases of the disease, there is bilateral symmetrical thalamic involvement. Abnormal signals on MRI are hypointense on T1 and hyperintense on T2. Restricted diffusion of the involved regions can be seen, often with the characteristic trilaminar sign 7,12. These findings can be quite extensive. Haemorrhage, cavitation, and post-contrast enhancement are also seen. MR spectroscopy can show elevated lipid/lactate and glutamine/glutamate peaks 11.
Treatment and prognosis
Acute necrotising encephalitis carries a very poor prognosis; the mortality rate is near 70%. Treatment is mainly supportive, as the precise aetiology remains unknown.
Differential diagnosis
If characteristic symmetric imaging findings are present, the differential diagnosis is limited. Lactic acidosis is not a classic finding of acute necrotising encephalitis. Otherwise, the differential diagnoses include:
-
associated with hypoglycaemia, hyperammonaemia and lactic acidosis
-
associated with hypoglycaemia, hyperammonaemia and lactic acidosis
viral encephalitides such as Japanese encephalitis or dengue encephalitis
Clinically, acute necrotising encephalitis may be differentiated from acute disseminated encephalomyelitis by an early onset of encephalitic features just after the prodromal illness while they may take 1 to 2 weeks to develop in acute disseminated encephalomyelitis.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.