Acute sinusitis (rare plural: sinusitides) is an acute inflammation of the paranasal sinus mucosa that lasts less than four weeks and can occur in any of the paranasal sinuses. If the nasal cavity mucosa is also involved (i.e. rhinitis), then the term rhinosinusitis is appropriate. Imaging is not routinely recommended in uncomplicated acute (rhino)sinusitis 13.
On this page:
Diagnosis
The American Academy of Otolaryngology-Head and Neck Surgery defines acute rhinosinusitis as ≤4 weeks of purulent nasal drainage with nasal obstruction and/or facial pain/pressure/fullness (including headache) 13.
Clinical presentation
Acute sinusitis typically presents with fever, headache, postnasal discharge of thick sputum, nasal congestion and an abnormal sense of smell 11.
Pathology
Aetiology
Acute sinusitis usually occurs following a viral upper respiratory tract infection. Dental caries, periapical abscess and oroantral fistulation may lead to a spread of infection to the maxillary sinus. Cystic fibrosis and allergy are risk factors.
Other anatomical variants that may predispose to the inflammation include nasal septal deviation, a spur of the nasal septum and/or frontoethmoidal recess variants.
Critical care patients
Patients in an intensive care setting are at an increased risk of acute sinusitis.
Risk factors identified include 10:
-
indwelling nasogastric and/or endotracheal tubes
especially nasotracheal routing
prolonged admission
younger age
Radiographic features
Imaging should be reserved for when a complication is suspected or an alternative diagnosis is being considered 13. Plain radiographs (x-rays) are not recommend with CT the first-line imaging test 13.
Imaging findings of acute sinusitis are non-specific and can be seen in a large number of asymptomatic patients (up to 40%) 11. An air-fluid level is the most typical imaging finding. However, it is only present in ~37.5% (range 25-50%) of patients with acute sinusitis 4.
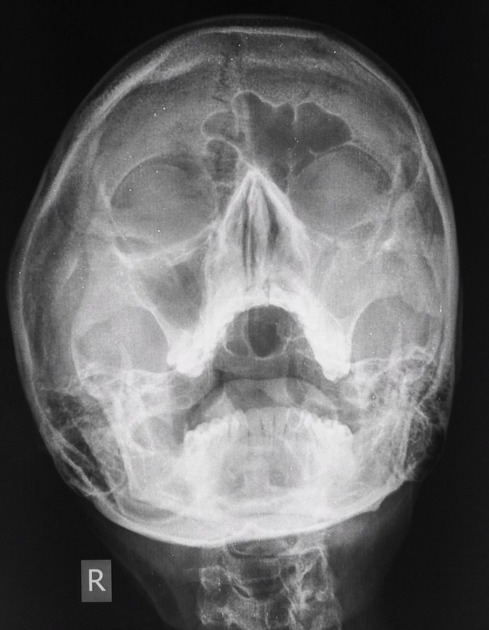
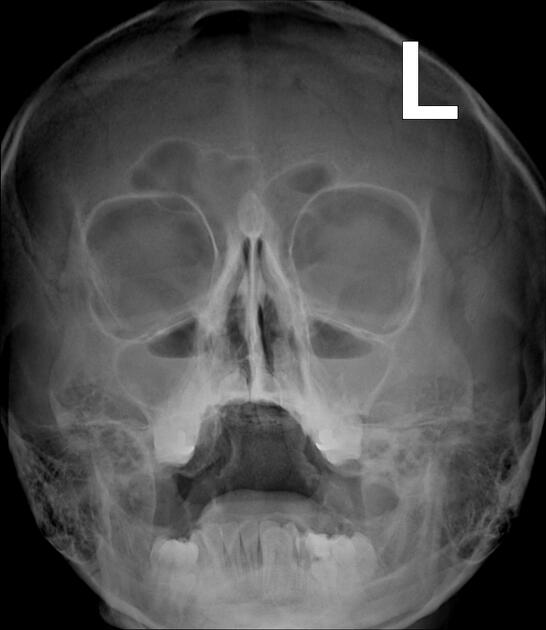
Plain radiograph
Sinus x-rays do not allow assessment of the extent of the inflammation and its complications. Opacification of the sinuses and gas-fluid level best seen in the maxillary sinus. Ethmoidal and sphenoidal sinuses are difficult to assess on plain radiography.
Ultrasound
Although not the primary mode of investigation, sonography may be used to screen for maxillary sinusitis; the perturbation of the normal air/fluid ratio in sinusitis alters the acoustic impedance of the usually aerated space. Normal and abnormal maxillary sinus features may be differentiated as follows:
-
normal maxillary sinus
a series of horizontal reverberation artifacts extend into the far-field, diminishing with each successive iteration, parallel to the prominent near field linear echogenic cortex of the maxilla 9
the far-field is ill-defined, and the posterior wall of the sinus is not visible
-
abnormal maxillary sinus
-
complete sinusogram 5
sagittal insonation reveals the absence of horizontal reverberation artifacts, replaced by an anechoic space
posterior wall appears in the far-field as an echogenic stripe
transverse insonation reveals this echolucent space bordered by the medial and lateral walls
this indicates the sinus is fluid-filled and is highly suggestive of sinusitis in the appropriate clinical context
-
partial sinusogram
sagittal visualisation of a portion of the posterior wall, with adjacent horizontal reverberation artifacts
medial/lateral walls obscured
-
nonspecific finding, but increased specificity if partial sinusogram present while semi-supine and absent when supine 6
this indicates an air-fluid level and is considered positive for sinusitis
presence when both semi-supine and supine thought to be indicative of mucosal thickening 7
-
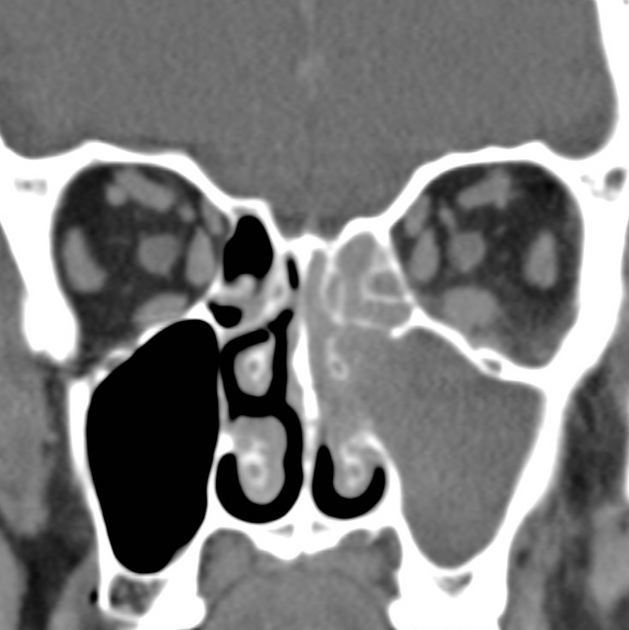
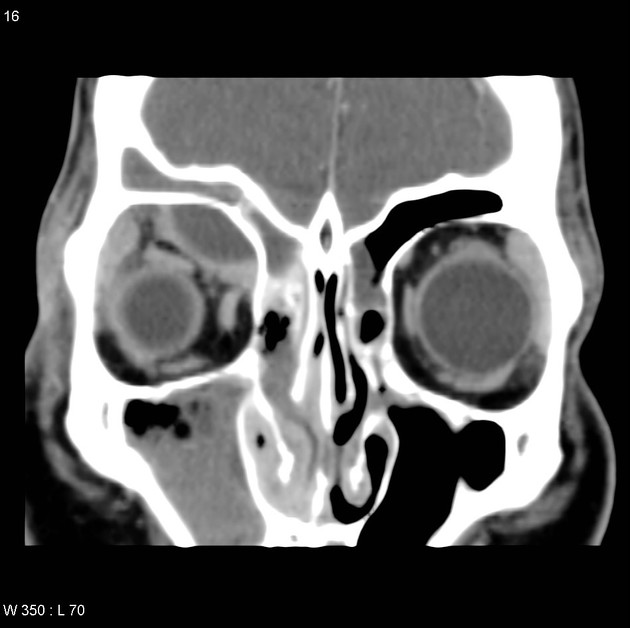
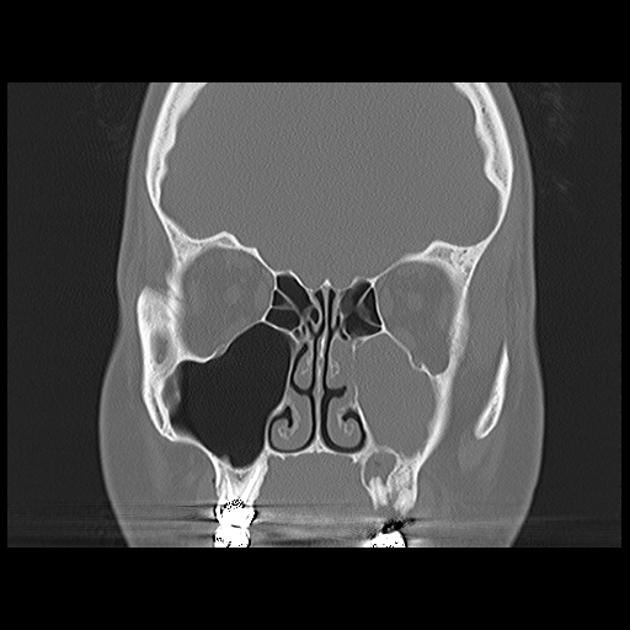
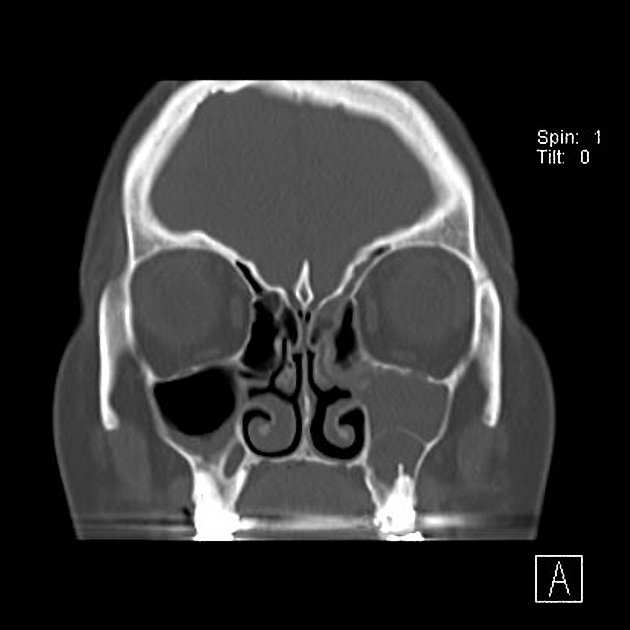
CT
CT is the most common method of evaluation but should be reserved for when a complication is suspected or an alternative diagnosis is being considered 13.
Described findings of the paranasal sinuses include
opacification 13
moderate-to-severe mucosal thickening 13
air-fluid levels 13
gas bubbles within the fluid / bubbly secretions
obstruction of the ostiomeatal complexes
Rhinitis, often associated with sinusitis, is often characterised by thickening of the turbinates with obliteration of the surrounding air channels. This should not be confused with the normal nasal cycle ref.
The fat pads surrounding the sinuses should be assessed for extra-sinus extension of disease ref, e.g. the retromaxillary fat posterior to the maxillary sinus.
The maxillary dentition should also be assessed as ~20% of maxillary sinus infections are odontogenic 11.
MRI
MRI is largely reserved for assessing complications of acute (rhino)sinusitis. 13
Signal characteristics
T1: mucosal thickening is isointense to soft tissue and fluid is hypointense
T2: both mucosal thickening and fluid are, to a variable degree, hyperintense
T1 C+ (Gd): inflamed mucosa enhances whilst fluid does not
Treatment and prognosis
Acute sinusitis is usually treated conservatively with medical treatment (e.g. analgesia, intranasal steroids, nasal irrigation 13) until the inflammation subsides +/- treatment of the cause, e.g. dental caries. If it becomes chronic sinusitis, functional endoscopic sinus surgery (FESS) may be considered.
Complications
-
erosion through bone
-
frontal sinus superficially (Pott puffy tumour)
frontal or ethmoidal sinuses into the orbit (subperiosteal abscess of the orbit)
-
-
intracranial extension









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.