Adrenal vein sampling (AVS) is a procedure where blood is collected from the adrenal veins via a catheter to confirm autonomous hormone production (usually aldosterone), if it is unilateral or bilateral, and to guide further treatment 1.
If unilateral, the adrenal gland can be removed; thus curing secondary hypertension in 50 to 80% of the cases that are caused by aldosterone-producing adenoma while the remaining cases show improvement in hypertension treatment 1. If bilateral, the hypertension is better controlled medically with aldosterone antagonists 1.
On this page:
Indication
Adrenal vein sampling is commonly performed in the workup of primary aldosteronism (PA), specifically to diagnose bilateral or unilateral production of excessive aldosterone (with or without discrete adrenal lesion).
Less commonly, AVS is performed to identify biochemically proven phaeochromocytoma when not visible on CT or other imaging methods 1. In rare occasions, adrenal vein sampling could be used for adrenal Cushing disease or for syndromes of androgen excess 1.
Pre-procedural assessment
Multiphase CT utilising an adrenal protocol is performed in patients with PA to 4:
identify a fat-poor adrenal adenoma that can mimic an aldosterone-secreting adenoma
identify adrenal cortical adenocarcinoma (rare cause of PA)
-
assess the (middle) adrenal veins and identify venous variants relevant to the catheter approach e.g. a right adrenal vein originating from or close to an accessory hepatic vein
the right adrenal vein arises directly from the posterior wall of the IVC at T12 level
the left adrenal vein in most cases unites with the inferior phrenic vein, forming a common trunk which drains into the left renal vein
Technique
Although technique varies a standard modern approach would consist of 1,3:
review of prior imaging cross-sectional
obtain venous access via common femoral vein (usually right) puncture with guiding catheter / microcatheter set-up
placement of selective catheter or sheath in the IVC or common femoral vein
-
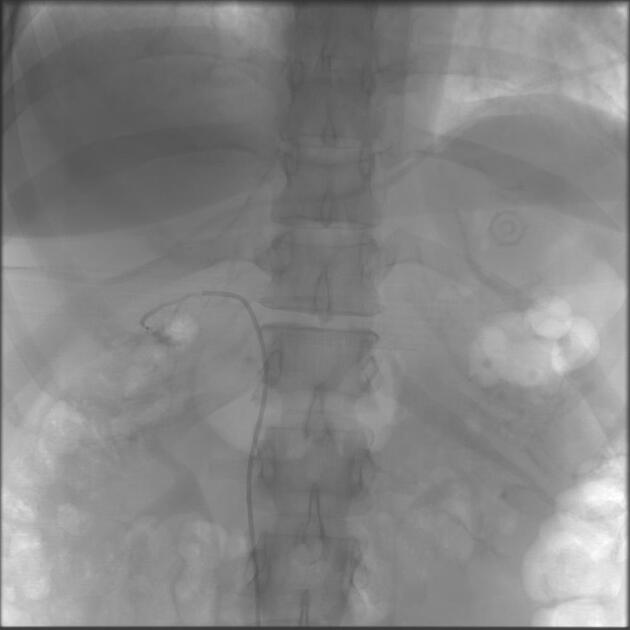
sequential cannulation of the adrenal veins - confirming position with contrast
back pain may be reported by the patient while contrast is injected into adrenal vein, particularly on the right
-
venous sampling from each adrenal vein and peripheral source (e.g. femoral vein)
some institutions use adrenocorticotropic hormone (ACTH) infusions before and during adrenal sampling
other institutions avoid it due a suspicion of possible misdiagnosed bilateral cases 1
-
it may be difficult to aspirate blood from the adrenal vein, likely due to suction causing vessel wall collapse at the catheter tip. Strategies to overcome this include
use of a catheter with a single side-hole close to the tip
intermittent gentle suction
suction using a partially air-filled syringe in order to reduce suction pressure
label all tubes (attention to right vs. left)
submit samples for laboratory assays (aldosterone and cortisol)
Complications
-
unrecognised failure to select the adrenal vein.
this is most common on the right, where an accessory hepatic vein can mimic the right adrenal vein
the right adrenal gland has a variable appearance on venography
identification of emissary veins from its capsule provides increased confidence for correct vein selection
in addition, contrast injection into an adrenal vein often produces discomfort, whereas contrast injection into an accessory hepatic vein will not 1
-
adrenal vein rupture due to contrast injection
reported incidence is 4-10%
in rare causes this can lead to adrenal haemorrhage, manifested clinically by severe pain which can persist for 2-3 days, and potentially causing permanent destruction of the gland 1
other complications include groin haematoma, vasogal response, intraprocedural back pain, infarction, adrenal vein thrombosis and perforation, hypertensive crisis, and adrenal insufficiency 1
Assessment of success
Assessment of successful AVS is not via venography, but rather hormonal analysis of samples. As the concentration of adrenal hormones decrease exponentially as distance from the adrenals increases, measurement of success is assessed by way of cortisol analysis 5.
The selectivity index (SI) is calculated by dividing the concentration of cortisol in the adrenal vein by the concentration in the IVC or femoral vein sheath. Thresholds for success vary according to institution.
The Australian and New Zealand AVS Working Group recommends for AVS that is not stimulated by ACTH infusion, an SI >2 is an acceptable cut off for successful adrenal vein cannulation 5. Regarding ACTH stimulated AVS however, an SI of greater than >5 was recommended although is is acknowledged that some authors consider an SI >3 to be satisfactory.
This heterogeneity has implications in assessment of success rates of AVS across institutions but also but also clinically. One study found that a more liberal cutoff lead to a higher rate of unilateral primary aldosteronism being diagnosed on AVS 6. Interestingly, a lower cure rate has been reported in operative patients who were diagnosed with a more lax SI cutoff 6.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.