Antiphospholipid syndrome (APS or APLS), also known as Hughes syndrome, is a systemic autoimmune disorder. It is usually defined as the clinical complex of vascular occlusion and ischemic events occurring in patients with circulating antiphospholipid antibodies.
On this page:
Clinical presentation
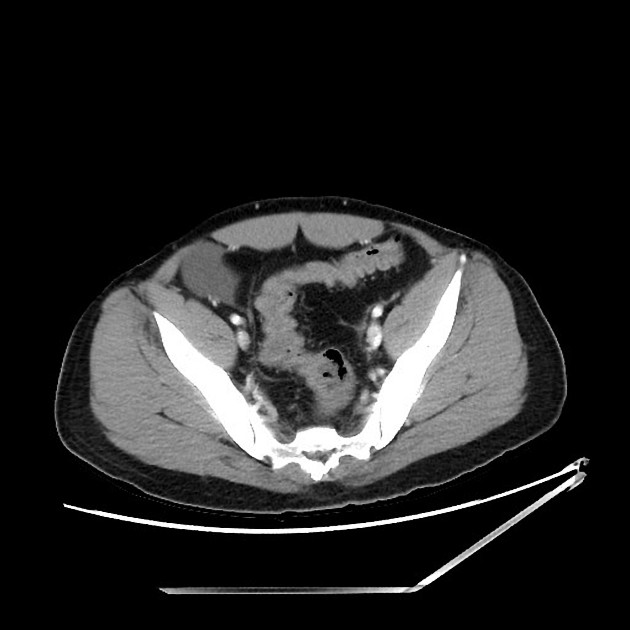
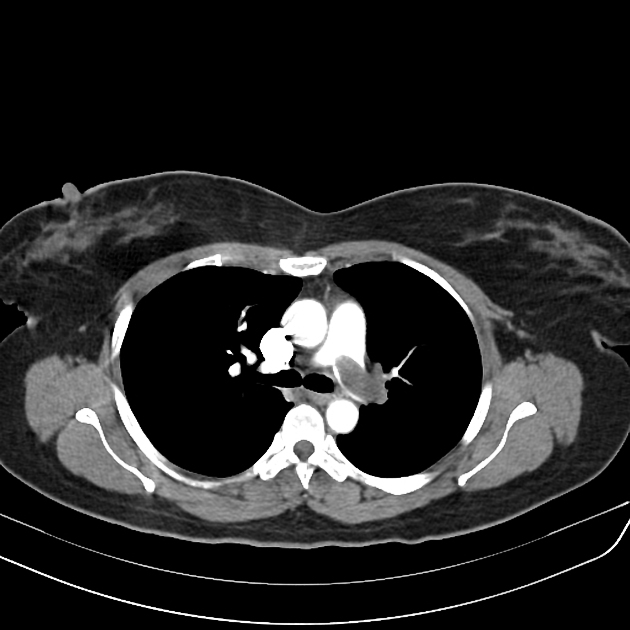
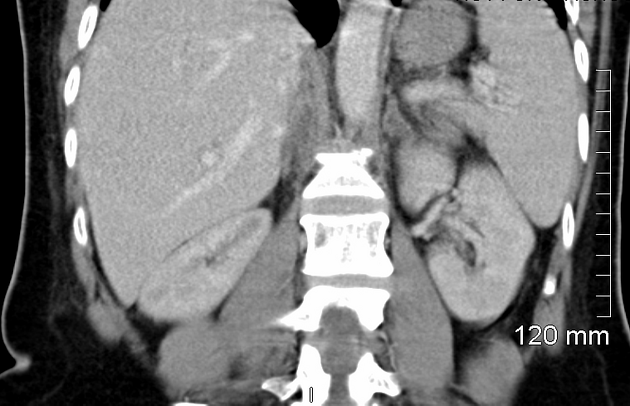
Antiphospholipid syndrome is characterized by venous, arterial, or small vessel thrombosis, potentially affecting multiple organ systems:
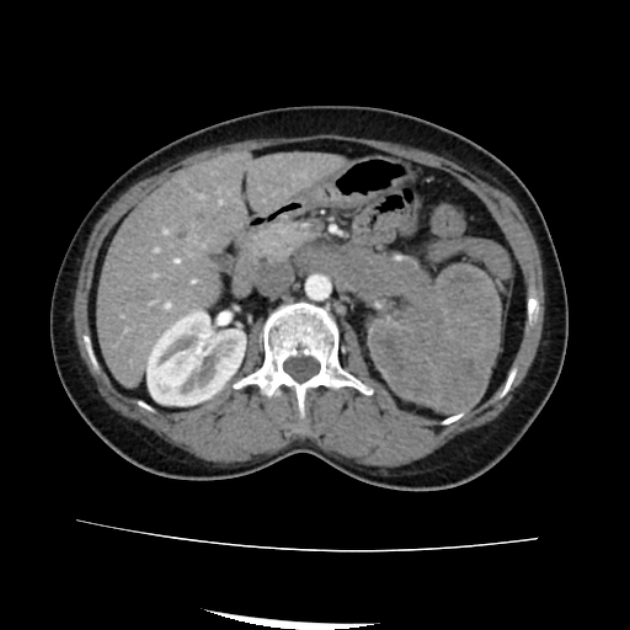
abdominal manifestations, e.g. renal vein thrombosis, Budd-Chiari syndrome, mesenteric ischemia
-
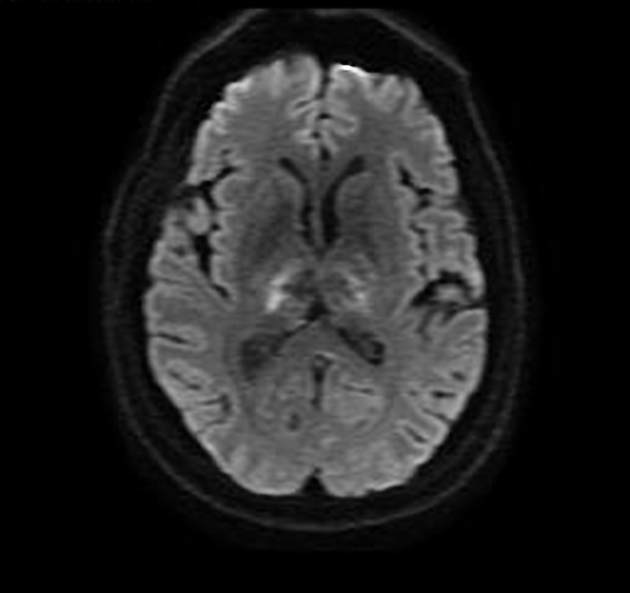
neurological manifestations 10
-
thrombotic-related: e.g. ischemic stroke, transient ischemic attack, cerebral venous thrombosis, etc.
if ischemic stroke is present with livedo reticularis, is sometimes known as Sneddon syndrome
non-thrombotic-related: e.g. movement disorders (e.g. chorea), transverse myelitis, headache, seizures, dementia, etc.
-
cutaneous manifestations, e.g. livedo reticularis, livedo racemosa
-
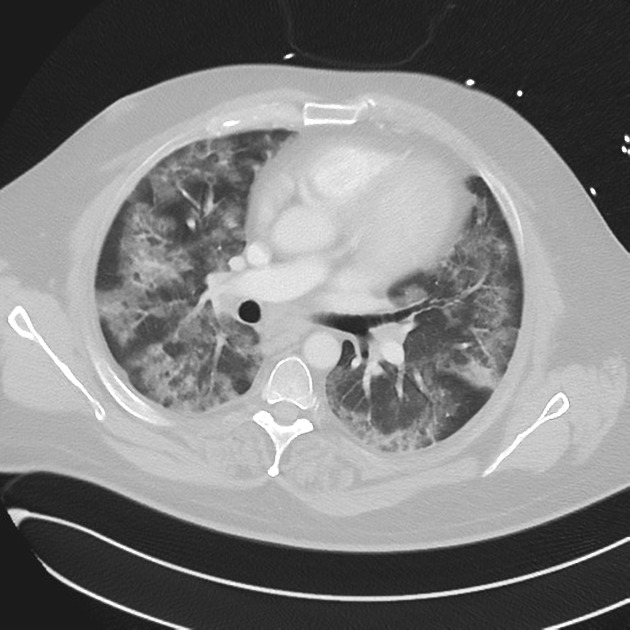
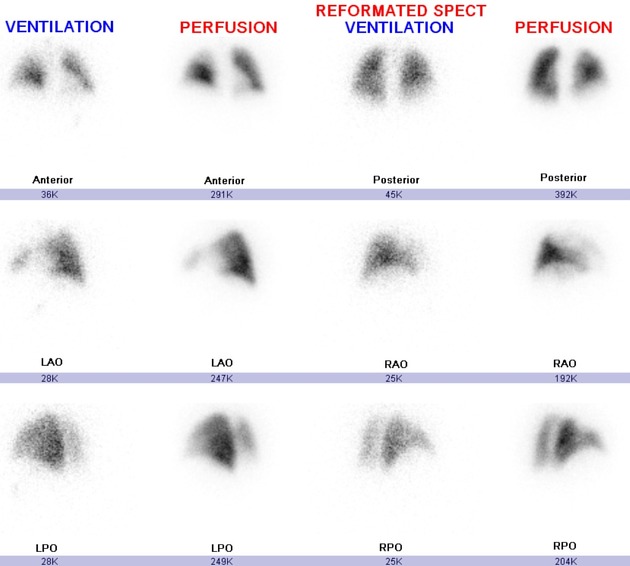
pulmonary manifestations, e.g. pulmonary embolus, diffuse alveolar hemorrhage
cardiac manifestations, e.g. valvular thickening
Pathology
Patients have circulating antiphospholipid antibodies that cross-react with cell membrane phospholipids. This results in a hypercoagulable state leading to vascular thrombosis.
Etiology
The disorder can be primary (primary antiphospholipid syndrome) or secondary, i.e. associated with systemic lupus erythematosus.
Markers
Positive lupus anticoagulant, anticardiolipin antibodies, and anti-beta2-glycoprotein I antibodies are seen but are not specific for antiphospholipid syndrome if considered in isolation (see diagnostic criteria below) 6. Paradoxically, if lupus anticoagulant is present, a patient's coagulation profile will show an elevated aPTT suggesting a propensity to bleeding, however this is not the case.
Diagnosis
Diagnosis is made using the revised Sapporo criteria, in which patients need to meet at least one clinical and at least one laboratory criteria to fulfill the diagnosis of antiphospholipid syndrome 7.
-
clinical criteria 7:
-
vascular thrombosis: ≥1 episode of venous, arterial, or small vessel thrombosis in any tissue or organ
superficial thrombophlebitis does not meet this criterion
pregnancy morbidity: 3 miscarriages <10 weeks, or 1 miscarriage ≥10 weeks, or premature birth before 34 weeks
-
-
laboratory criteria (detected on ≥2 occasions on testing at least 12 weeks apart) 7:
anticardiolipin antibodies
anti-beta2-glycoprotein I antibodies
lupus anticoagulant
Treatment and prognosis
Asymptomatic antiphospholipid syndrome does not warrant any antiplatelet or antithrombotic therapy 8. However, warfarin is used for acute thromboembolic events or as secondary prevention 8. Management of organ-specific manifestations of antiphospholipid syndrome are beyond the scope of this general article. Less than 1% of patients develop the more serious and fatal catastrophic antiphospholipid syndrome.
History and etymology
The condition was first described by Graham RV Hughes, English rheumatologist, and colleagues in 1983 9.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.