Ascites (hydroperitoneum is a rare synonym) is defined as an abnormal amount of intraperitoneal fluid.
On this page:
Terminology
Ascites (plural is the same word) tends to be reserved for relatively sizable amounts of peritoneal fluid. The amount has not been defined formally. It is noted physiologically, however, that there is approximately 50-75 mL of fluid within the peritoneal space in normal patients. When only a small amount of fluid is present, which may be physiological, radiologists tend to use the term "free peritoneal fluid" or "free fluid" instead.
Occasionally, the term "trace ascites" might be employed. It has been pointed out that the term free fluid would seem not to include small amounts of loculated fluid, as 'free' and 'loculated' are antonymic 11,12.
Clinical presentation
Patients with a large volume of ascites can present with abdominal distension (which may be painful), nausea, vomiting, dyspnea, and peripheral edema 7,9.
Pathology
Ascitic fluid is traditionally characterized as either:
transudate: thin, low protein count and low specific gravity
exudate: high protein count and high specific gravity
The concept of the serum-ascites albumin gradient has been shown to be more accurate in the classification of the causes of ascites 5. For the purposes of simplicity, however, we maintain the former classification.
Colors of ascitic fluid may suggest the following conditions:
bloody: traumatic tap, hepatocellular carcinoma, peritoneal carcinomatosis
cloudy or turbid: spontaneous bacterial peritonitis, pancreatitis
milky: tuberculosis, malignancy
clear or straw color: cirrhosis, congestive cardiac failure 13
dark brown: biliary perforation or leak 14
Etiology
Causes of transudative ascites:
peritoneal dialysis, i.e. continuous ambulatory peritoneal dialysis (CAPD)
-
malignancy (~10% of refractory ascites) 7,9
most commonly: breast, ovarian, endometrial, gastrointestinal and pancreatic 7
Causes of exudative ascites:
peritonitis, e.g. tuberculosis
Radiographic features
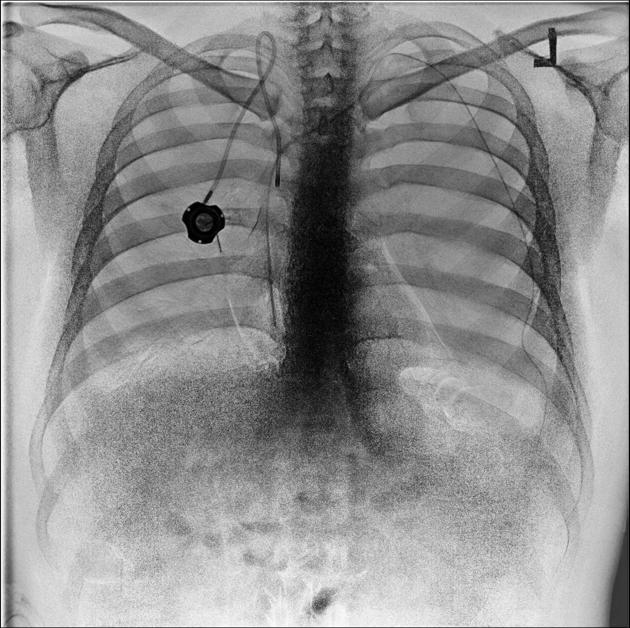
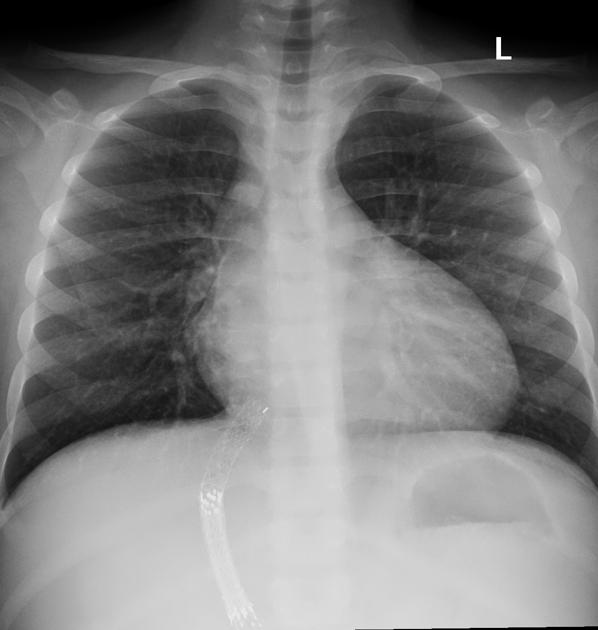
Plain radiograph
Detection of intraperitoneal fluid on a plain radiograph requires at least 500 mL to be present.
Plain radiograph findings of ascites include:
diffusely increased density of the abdomen
poor definition of the soft tissue shadows, such as the psoas muscles, liver and spleen
medial displacement of bowel and solid viscera (away from the properitoneal fat stripe)
bulging of the flanks
increased separation of small bowel loops
dog ear sign: represents fluid in pelvic peritoneal recess 10
Ultrasound
May detect smaller volumes especially if they are adjacent to the diaphragm or anterior margin of the liver 3. Assessment of fluid type:
simple ascites is anechoic
exudative, hemorrhagic or neoplastic ascites contains floating debris
septations suggest an inflammatory or neoplastic cause and may be called a loculated ascites
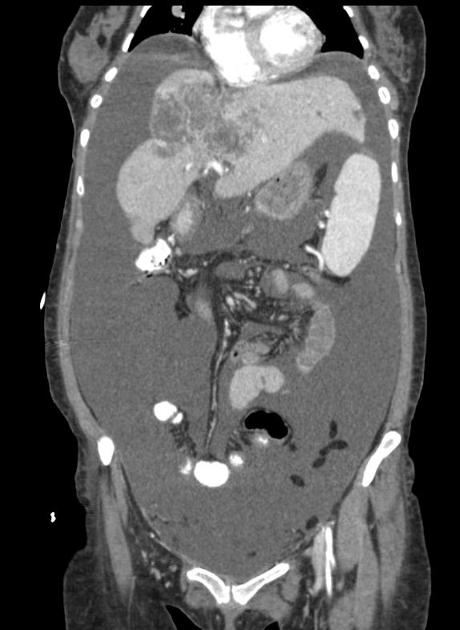
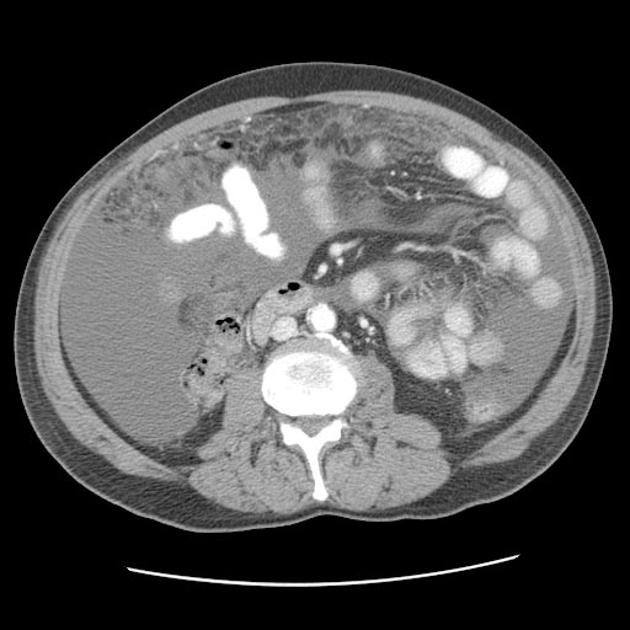
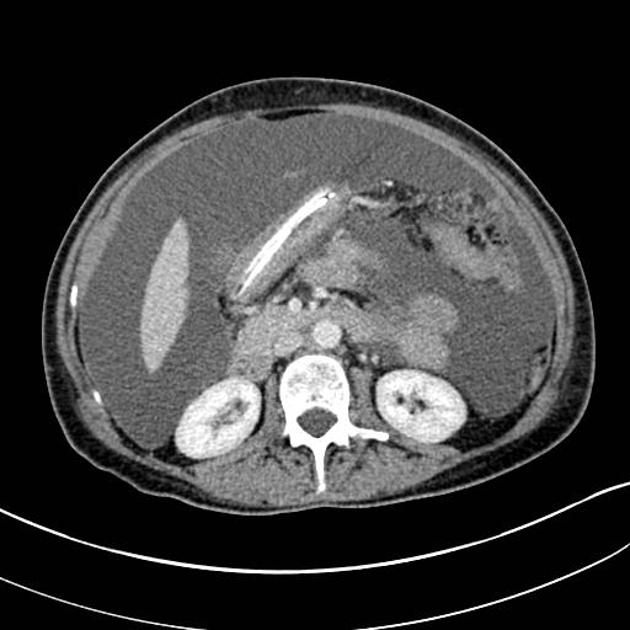
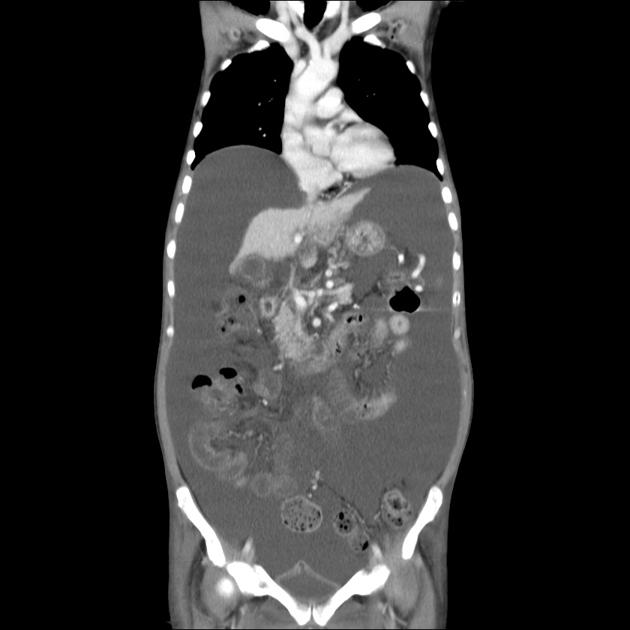
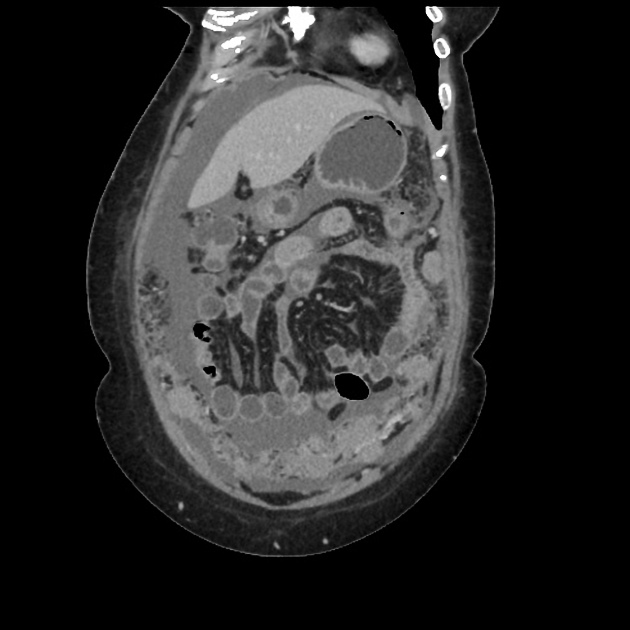
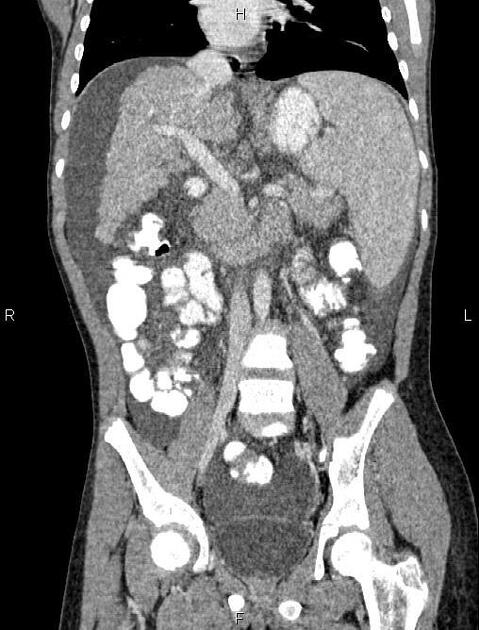
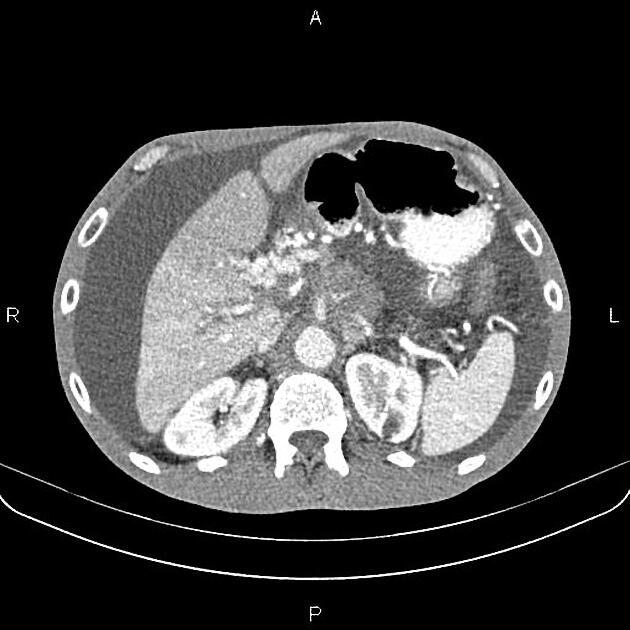
CT
CT is most sensitive to small amounts of fluid in the peritoneum which collects preferentially in the dependent regions, such as Morison's pouch and the pelvis. The CT density of intraperitoneal fluid may give a clue to the underlying etiology:
transudative ascites density should be approximate to that of water (-10 to +10 HU)
exudative ascites (density >15 HU)
hemoperitoneum density is higher still (~45 HU)
Of course, other intra- or extra-abdominal CT features may give further evidence to the origin of the ascites, e.g. features of heart failure, features of cirrhosis, peritoneal catheter in situ, etc.
Treatment and prognosis
Medical management includes a modified diet (restricting sodium) and the use of medications such as diuretics 7,9.
Interventional techniques for management include serial paracentesis (ascitic tap), transjugular intrahepatic portosystemic shunt (TIPS) or peritoneovenous shunting 8,9.
Ascitic taps are the most common and thought to be the most effective treatment for symptomatic ascites 9. It can be performed with a variety of techniques depending on the institution and the availability of imaging resources 8:
blind: i.e. non-imaging guided
partially imaging-guided: an appropriate site is marked on the abdominal wall using ultrasound but the puncture is blind
imaging-guided: usually using ultrasound
Differential diagnosis
Consider other causes of intraperitoneal fluid:
physiological: small amount of pelvic fluid may be normal in young females
choleperitoneum: biloma/bile leak, e.g. from cholecystectomy
uroperitoneum: urinoma/urine leak, e.g. from bladder trauma









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.