Astroblastomas are rare glial tumors usually found in the cerebral hemispheres of young adults and children.
On this page:
Terminology
The exact nature of astroblastomas remains to be fully elucidated. Tumors with compatible histological features have a variety of molecular characteristics and overlap with other better-known tumors such as pleomorphic xanthoastrocytomas or ependymomas or diffuse astrocytomas 6,7.
The presence of MN1 alterations (a transcriptional coregulator involved in the development of acute myeloid leukemia and meningiomas) is now used to define the lesion, and thus it is now named astroblastoma, MN1-altered and considered circumscribed astrocytic gliomas in the 5th edition (2021) WHO classification of CNS tumors 6.
Epidemiology
They occur at all ages, ranging from early childhood to the sixth decade but are most commonly seen in children, adolescents, and young adults with a mean age between 10-30 years 2,5. A strong female predilection has been suggested in some reports 5,6.
Pathology
Astroblastomas have not yet been given a WHO grade, but do have a range of histological appearance and biological behavior ranging from relatively indolent (astroblastoma) to aggressive (anaplastic or malignant astroblastoma) 4,5.
Macroscopic appearance
They are well-demarcated masses with areas of cystic degeneration and necrosis giving it a bubbly appearance. Hemorrhages and adjacent brain infiltration are rare.
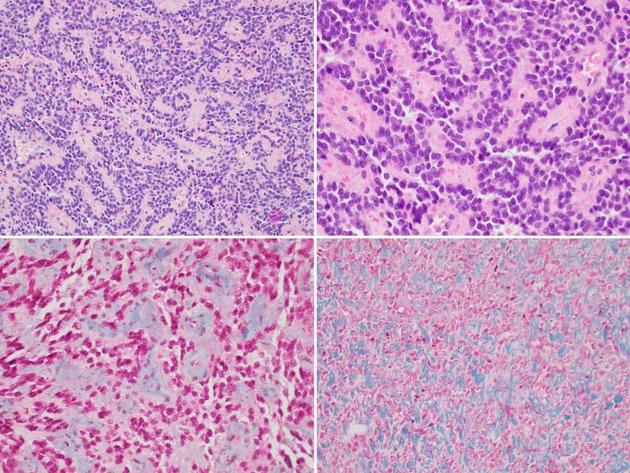
Microscopic appearance
Astroblastomas have elongated glial cells with abundant eosinophilic cytoplasm and a broad, or “stout”, GFAP positive process extending radially towards a central blood vessel, forming "astroblastic pseudorosettes", reminiscent to the perivascular pseudorosettes of ependymomas, which are a characteristic feature of this tumor. The central vessel tends to be hyalinized.
Although no agreed-upon criteria have been accepted, anaplastic/malignant histological features include 5:
increased mitotic activity (>5 mitoses per 10 high-powered fields)
high cellularity
anaplastic nuclear features
microvascular proliferation
palisading necrosis
usually Ki-67 >10%
Immunophenotype
Radiographic features
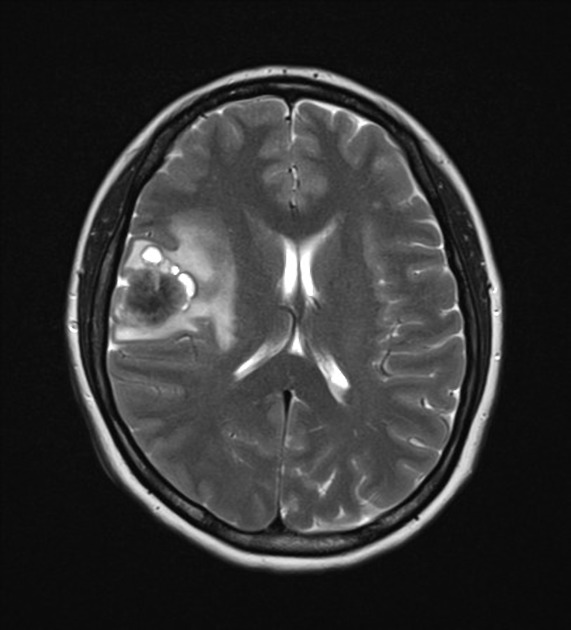
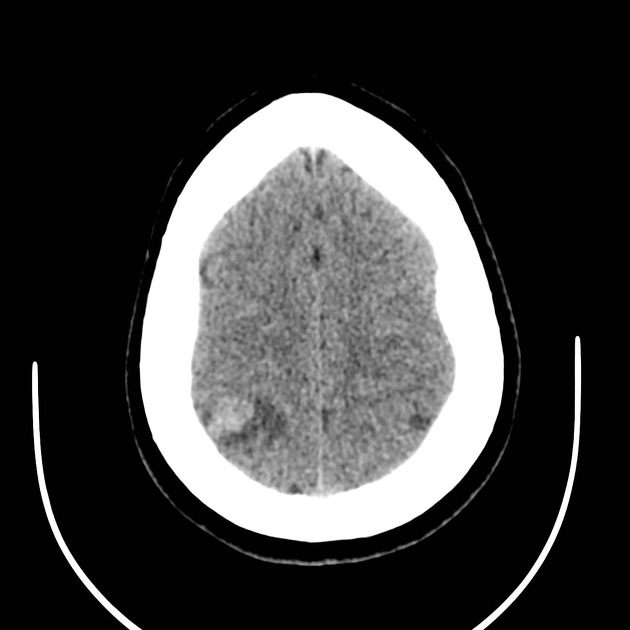
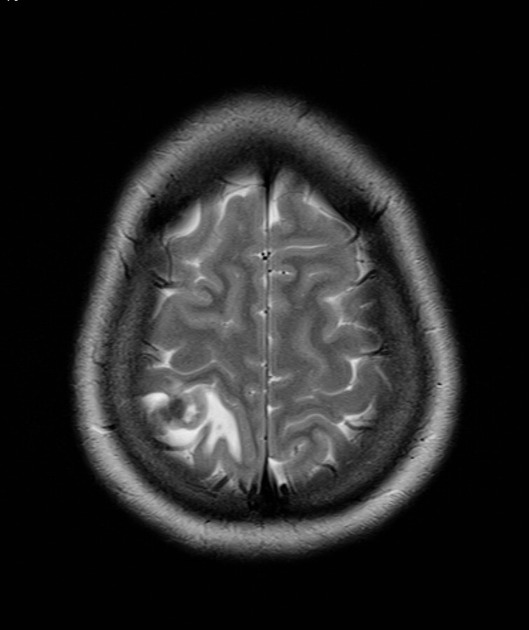
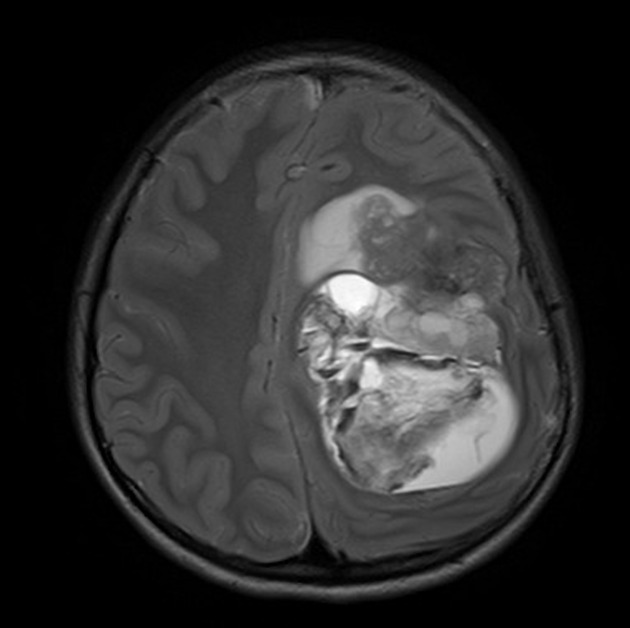
Astroblastomas are usually fairly sizable, peripherally located, supratentorial lobulated solid cystic masses with little if any associated vasogenic edema 1-5. Multiple cysts are common and can give it a bubbly appearance. Calcification is very common and seen in 85% of cases, and usually in a punctate pattern.
MRI
Reported signal characteristics include 2:
T1: iso- to hypointense
-
T2/FLAIR
heterogeneous with a multicystic or bubbly appearance
solid components tend to be isointense to grey matter
relatively little surrounding edema compared to size
T1 C+ (Gd): heterogeneous enhancement
-
DWI/ADC
facilitated diffusion in fluid/cystic components
intermediate ADC values of the solid component (1190 to 1250 x 10-6 mm2/s) 8
Treatment and prognosis
Surgical resection is the treatment of choice with adjuvant radiation therapy and chemotherapy reserved for high-grade lesions. Recurrence after complete surgical resection of low-grade tumors is uncommon 4.
Differential diagnosis
Possible imaging differential considerations include:
astrocytoma, particularly GBM or gemistocytic
-
nodular calcifications instead of punctate calcifications 2




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.