Azoospermia refers to complete absence of sperm in the semen. It accounts for 5-10% of male infertility 1.
On this page:
Pathology
It can be obstructive or non-obstructive, e.g. primary testicular failure. This differentiation is of utmost importance, as obstructive azoospermia can be corrected by surgical intervention 1,2.
Aetiology
Obstructive azoospermia
congenital bilateral absence of ductus (vas) deferens (CBAVD)
obstruction of ductus (vas) deferens
inflammatory lesion of epididymis or ductus deferens
inflammatory obstruction of ejaculatory duct
iatrogenic injury (vasectomy, hernia repair, etc.)
varicocele (controversial if it causes azoospermia)
Non-obstructive azoospermia (primary testicular failure)
Y microdeletion
unexplained testicular failure
Radiographic assessment
Ultrasound
Scrotal ultrasound
Sonographic features that may be present with azoospermia include:
ectasia of rete testes: anechoic tubular structures in mediastinum testes
tubular ectasia of epididymis: multiple anechoic tubular structures in epididymal head (the differential for this feauture includes spermatocele, epididymal cyst)
inflammatory epididymal mass: enlarged heterogenous epididymis head
testicular volume: small sized testes (<7 mL) is seen in primary testicular failure. However, testicular volume is usually larger (>13 mL) in obstructive azoospermia 2.
Transrectal ultrasound
Sonographic features that may present on transrectal ultrasound include:
absence of ductus deferens
dilated ductus deferens (diameter >1.5 mm)
hypoplastic seminal vesicles (transverse diameter <7 mm and length <16 mm) 2,3
dilated seminal vesicles (transverse diameter >15 mm and length >25 mm) 2,3
inflammatory cyst(s) in ejaculatory duct
Fluoroscopy
Vasography (vasculodeferentography) has rare application now, however, theoretically stays the gold standard to evaluate obstructive azoospermia.
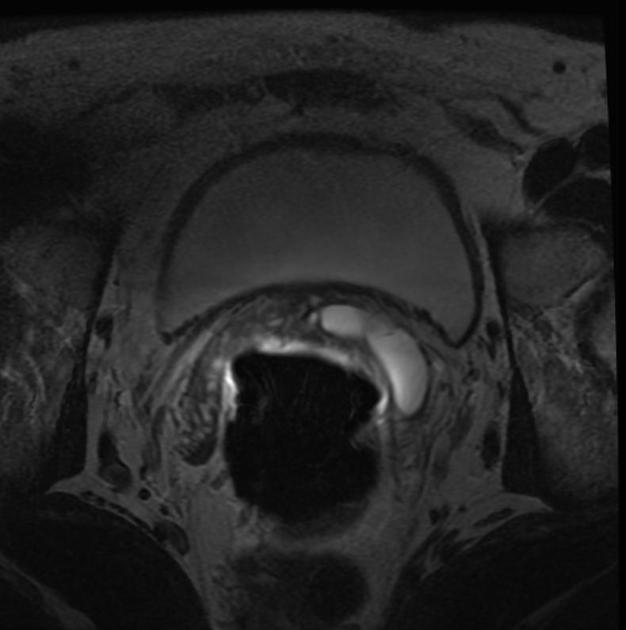
MRI
Similar features like absence or ductus deferens or seminal vesicle can be seen on MRI. Epididymal and seminal vesicle cysts can also be well seen. Endorectal MRI is the preferred modality.
Treatment and prognosis
Patients with primary testicular failure (non-obstructive azoospermia) benefit from intracytoplasmic sperm injection. Obstructive azoospermia patients benefit from surgical correction such as vasoepididymostomy. Also, we can obtain sperm directly from epididymis or seminal vesicle, in cases of obstructive azoospermia.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.