Basal ganglia haemorrhages are a common form of intracerebral haemorrhage, and usually result from poorly controlled long-standing hypertension, although they also have other causes. When due to chronic hypertension, the stigmata of chronic hypertensive encephalopathy are often present (see cerebral microhaemorrhages).
On this page:
Epidemiology
Basal ganglia haemorrhages are a subset of intracerebral haemorrhage yet account for 65% of spontaneous intracerebral haemorrhages 6.
Clinical presentation
The presentation will vary widely depending on the patient's medical history and the size of the haemorrhage. There is a strong association between basal ganglia haemorrhage and lacunar syndromes, for example, haematomas involving the posterior limb of the internal capsule will lead to contralateral motor deficits 7,8. Patients can present with an ipsilateral deviation of the eyes due to descending capsular pathways from the frontal eye field.
Pathology
Long-standing poorly controlled hypertension accounts for the majority of basal ganglia haemorrhage, and leads to a variety of pathological changes in the vessels:
-
microaneurysms of perforating arteries (Charcot-Bouchard aneurysms)
small (0.3-0.9 mm) diameter aneurysms that occur on small (0.1-0.3 mm) diameter arteries
-
a distribution that matches the incidence of hypertensive haemorrhages 5
80% lenticulostriate
10% pons
10% cerebellum
found in hypertensive patients
may thrombose, leak (see cerebral microhaemorrhages) or rupture 2
accelerated atherosclerosis: affects larger vessels
hyaline arteriosclerosis
hyperplastic arteriosclerosis: seen in very elevated and protracted cases
Radiographic features
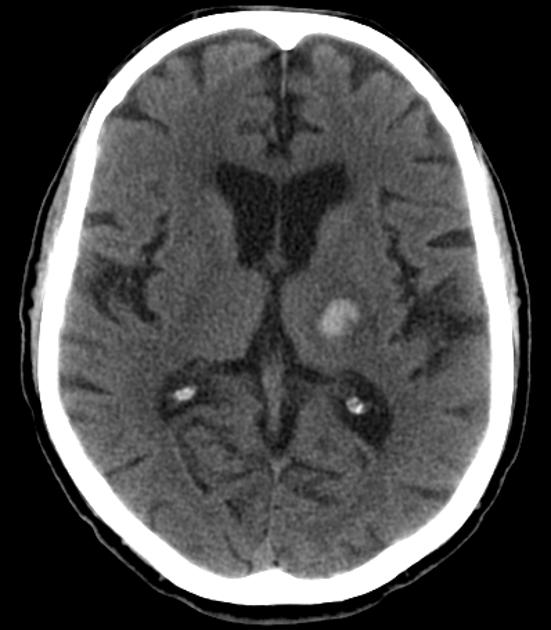
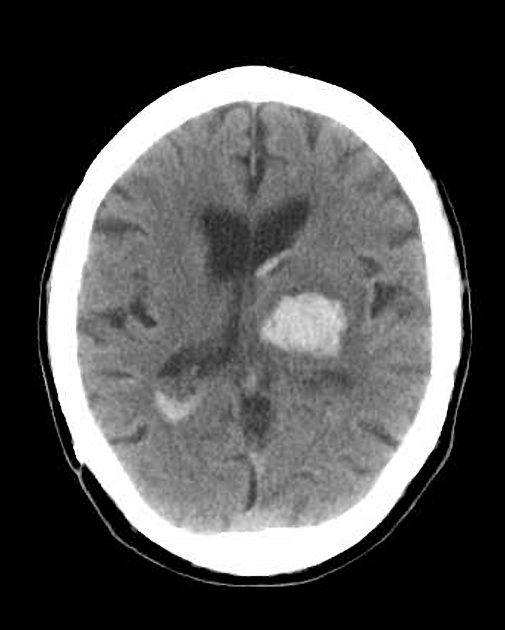
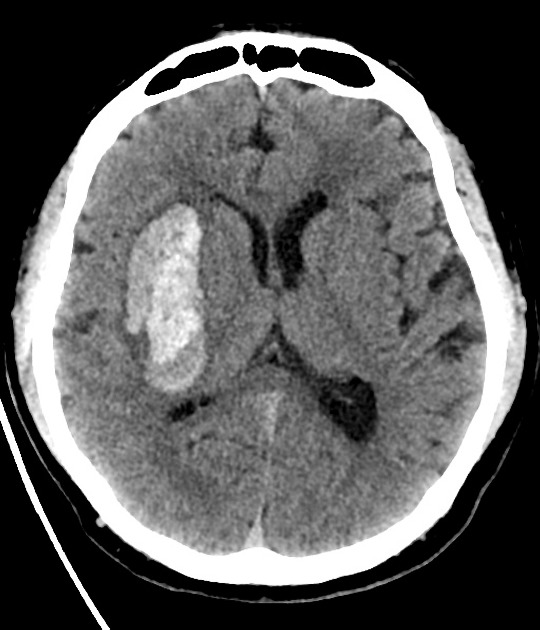
Neuroimaging demonstrates haemorrhage centred in the basal ganglia. There may be extension into the ventricles, with the parenchymal component occasionally being very small or inapparent. Rarely, there may be extension into the contralateral basal ganglia, possibly via the canal of Gratiolet 11,12.
CT
Haemorrhage is demonstrated as a region of hyperdensity in the basal ganglia. If there is no intraventricular extension, the haemorrhage volume may be estimated by ABC/2 and related formulas, which may have neurosurgical and prognostic implications.
There are many predictors of haematoma expansion potentially evident on CT, which are discussed in depth in the main intracerebral haemorrhage article.
MRI
The appearance of haemorrhage on MRI varies with time and to some degree the size of the haematoma (see ageing blood on MRI).
Treatment and prognosis
The mainstay of treatment is medical, and medical management does not differ for other causes of intracerebral haemorrhage - please see the article on intracerebral haemorrhage for further discussion 9. In selected patients, there may be a role for decompressive craniectomy 10.
If an intraventricular component to the haemorrhage is present then hydrocephalus is a common sequelae and CSF drainage with an external ventricular drain is often needed. Evacuation of the clot is controversial and without a strong evidence base.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.