Brenner tumours are an uncommon surface epithelial tumour of the ovary. It was originally known as a transitional cell tumour due to its histological similarity to the urothelium. Brenner tumours account for ~3% of ovarian epithelial neoplasms. They can very rarely occur in other locations, including the testis.
On this page:
Epidemiology
Most often found incidentally in women between their 5th and 7th decades of life.
Clinical presentation
They are most frequently found incidentally on pelvic examination or at laparotomy.
Pathology
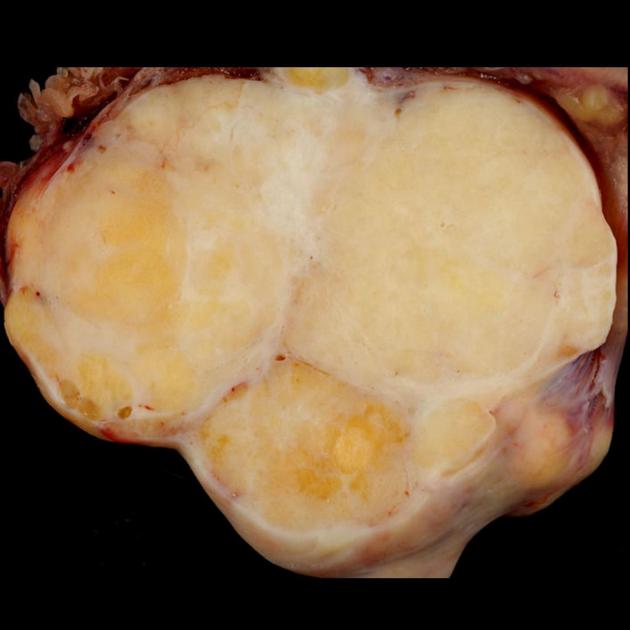
Histological specimens often show transitional cells covered by fibrous stroma, similar to neoplasms of the urothelium 8,9.
Associations
Brenner tumours are associated with another epithelial ovarian neoplasm of either the ipsilateral or contralateral ovary in ~30% of cases 6.
Location
Brenner tumours can be bilateral in 6-7% of cases.
Radiographic features
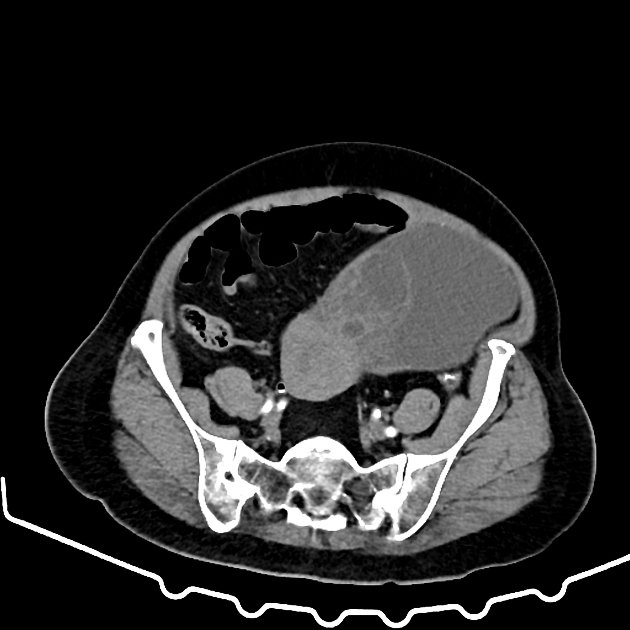
Often manifesting as a multilocular cystic mass with a solid component or as a mostly solid mass.
Tumours are usually small (<2 cm). Even with the occasional large tumour (>10 cm), there is often a lack of local invasion, lymphadenopathy, ascites, or metastases (i.e. peritoneal metastases, omental caking), which help distinguish it from other malignant ovarian neoplasms.
Pelvic ultrasound
Brenner tumours are similar to other solid ovarian neoplasms, particularly fibromas-thecomas, and can also be confused with pedunculated leiomyomas.
They are mainly hypoechoic solid masses. Calcifications have been reported in 50% of Brenner tumours on ultrasound.
CT
- calcifications have been reported in ~85% of Brenner tumours on CT
- the solid component may show mild to moderate enhancement post-contrast
MRI
- due to its predominantly fibrous content, they appear hypointense on T2-weighted sequences
Treatment and prognosis
Most Brenner tumours are benign.
Differential diagnosis
General imaging differential considerations include:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.