Cerebellar, hippocampal, and basal nuclei transient oedema with restricted diffusion (CHANTER) syndrome
Cerebellar, hippocampal, and basal nuclei transient oedema with restricted diffusion (CHANTER) syndrome describes a constellation of imaging findings in adults with opioid neurotoxicity. It is characterised by cytotoxic oedema in the bilateral hippocampi and cerebellar cortices, and variably in the basal ganglia 1.
On this page:
Terminology
CHANTER likely represents a severe form of acute opioid-induced neurotoxicity falling within a pathophysiologic spectrum that includes paediatric opioid use‐associated neurotoxicity with cerebellar oedema (POUNCE) syndrome (which occurs in children) and opioid-associated amnestic syndrome (which involves the hippocampi alone) 2. It is most commonly seen in the setting of fentanyl overdose 2.
It is, however, probably distinct from chasing the dragon leukoencephalopathy, which predominantly affects white matter and occurs after inhalational heroin use.
Clinical presentation
Patients present with a decreased level of consciousness 1,2.
Radiographic features
CT
CT primarily demonstrates cerebellar swelling and decreased attenuation due to oedema, with resultant obstructive hydrocephalus 1.
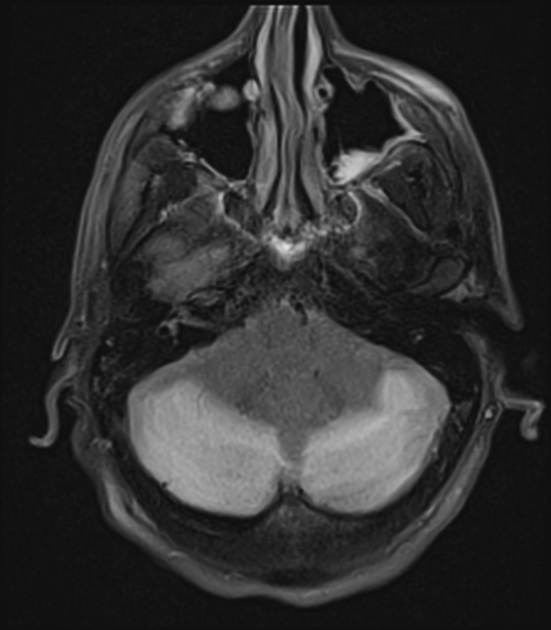
MRI
MRI is necessary to make the diagnosis as diffusion restriction is a key imaging feature.
In addition to cerebellar oedema, with or without obstructive hydrocephalus, MRI demonstrates bilateral, symmetric restricted diffusion in the grey matter of the cerebellum and hippocampi, as well as asymmetric involvement of the basal ganglia 1,2. Although initially the cerebral cortex was reported as being spared 1, subsequenly published cases do include occasional cortical involvement, particularly in the occipital poles 2. Subcortical white matter involvement is uncommon 1,2.
Treatment and prognosis
Importantly, unlike diffusion restriction seen in the setting of hypoxic ischaemic encephalopathy (HIE), which is generally considered irreversible and thus carried a poor prognosis, changes seen in CHANTER are largely reverible if mass effect and hydrocephalus can be successfully managed 1,2.
Thus, treatment focuses of management of posterior fossa mass effect due to cerebeller oedema and resultant hydrocephalus. Management may include 1,2:
osmotic therapy: manitol and/or hypertonic saline
extraventricular drain placement
posterior fossa decompression
Additionally, due to decreased level of consciousness, these patients are often intubated and mechanically ventilated 1.
Prognosis is dependent on the degree to which the above therapies are able to prevent brainstem compression and herniation. If successful some patients make a near-complete recovery whereas others remain debilitated by memory, motor and speech deficits 1,2.
History and etymology
The syndrome was first described by an American group of clinicians in a seminal case series in 2019 1.
Differential diagnosis
hypoxic-ischaemic encephalopathy can also cause restricted diffusion in the hippocampus, cerebellar cortex, and deep grey nuclei, but cerebral cortex should also be involved





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.