Conventional osteosarcomas (COS) are high-grade malignant bone-forming tumours typically arising within the medullary cavity of bone 1-3.
On this page:
Epidemiology
Conventional osteosarcoma is the most common subtype of osteosarcoma consisting of approximately 75-80% of all cases 1-4. It is most frequently seen in the 2nd decade and later with a smaller peak in the 5th decade of life. Men are more commonly affected 1.
Diagnosis
The diagnosis of conventional osteosarcomas is based on a combination of typical radiographic features and histology 1,2.
Diagnostic criteria
Diagnostic criteria according to the WHO classification of soft tissue and bone tumours (5th edition) 1:
imaging features of a bone tumour
permeative and destructive growth pattern
osteoid/bone production by tumour cells
location within the medullary cavity
The following criteria are desirable:
high-grade atypia of tumour cells
frequent atypical mitotic figures
Clinical presentation
The typical clinical presentation includes pain and a growing mass for weeks or months and sometimes restricted motion in the adjacent joint 1,5. Additional symptoms include erythema and warmth.
A small number of patients will present with a pathological fracture.
Complications
Complications include the following 1:
skip lesions and distant metastases (e.g. lung)
pathological fracture: ~10-15%
Pathology
Conventional osteosarcomas are predominantly intramedullary located osteoid-producing highly aggressive and malignant mesenchymal tumours associated with high mitotic activity and frequent tumour necrosis 1,2.
Aetiology
The exact aetiology of osteosarcoma and conventional osteosarcoma is unknown 1.
However, sporadic conventional osteosarcoma is characterised by chromosomal instability and there are a few rare syndromes with germline mutations in RECQ helicases associated with conventional osteosarcoma 1.
Location
Conventional osteosarcomas are usually found in the long bones of the extremities but can occur in any bone 1.
The most frequent locations are as follows 1,2,6:
distal femur: ~30%
proximal tibia: ~15%
proximal humerus: ~15%
jaws
axial skeleton
Within the long bones, the tumours arise usually from the metaphyses ~90%, infrequently from the diaphysis ~9% and only rarely from the epiphysis <1% 1.
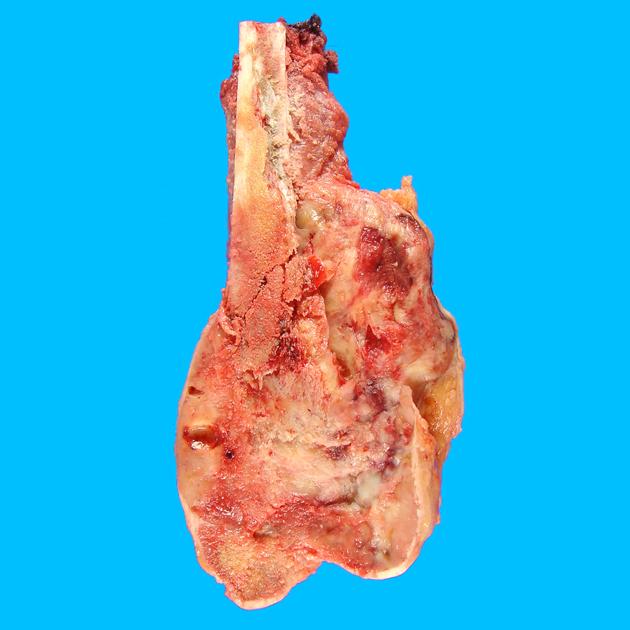
Macroscopic appearance
Macroscopically conventional osteosarcomas are characterised by the following features 1:
often a large intramedullary mass of the metaphyseal region
variable extension into the adjacent epiphysis or diaphysis
densely solid tan-white/yellow heavily mineralised components
grey and rubbery non-mineralised cartilaginous parts
areas of haemorrhage
areas of tumour necrosis
cystic change
eccentric circumferential soft tissue mass in the setting of soft tissue extension
possible displacement of the periosteum
Microscopic appearance
Microscopically, conventional osteosarcomas display a broad spectrum with the following histological features 1:
neoplastic bone formation (essential)
permeative growth pattern with erosion of preexisting trabeculae
new bone formation
severe anaplasia and pleomorphism
high mitotic activity
Based on their predominant histological pattern conventional osteosarcomas can be divided into the following subtypes 1-4,7,8:
osteoblastic: thin lace-like trabeculae to compact bone formation
chondroblastic: neoplastic hyaline cartilage merging with neoplastic bone
fibroblastic: predominantly spindled or less commonly epitheloid cells with extracellular collagen
Immunophenotype
On immunohistochemistry conventional osteosarcomas display a broad profile, but without any specificity. Frequently positive antigens include osteocalcin, osteonectin, osteoprotegerin, SATB2, RUNX2, S100, actin and CD99. Conventional osteosarcomas might be also positive for EMA and keratin 1.
Usually, tumours are negative for CD31, CD45 and FOS 1.
Radiographic features
Characteristic imaging features of conventional osteosarcoma include 1:
tumour mineralisation with an osteoid tumour matrix
permeative bone destruction
periosteal displacement with reactive new-bone formation with different patterns
extraosseous soft tissue extension
The osteoblastic subtype displays a more dense cloud-like mineralisation pattern whereas a more lytic radiographic appearance suggests fibroblastic or chondroblastic subtypes with unmineralized tissue components 8-10.
Plain radiograph
Characteristic appearances of conventional osteosarcoma on plain radiographs include the following 1,2,8-10:
osteolytic lesion
a wide, indistinct transition zone
non-expansile cortical destruction
aggressive periosteal reaction (sunburst, onion skin-like, Codman triangle)
increased soft tissue density
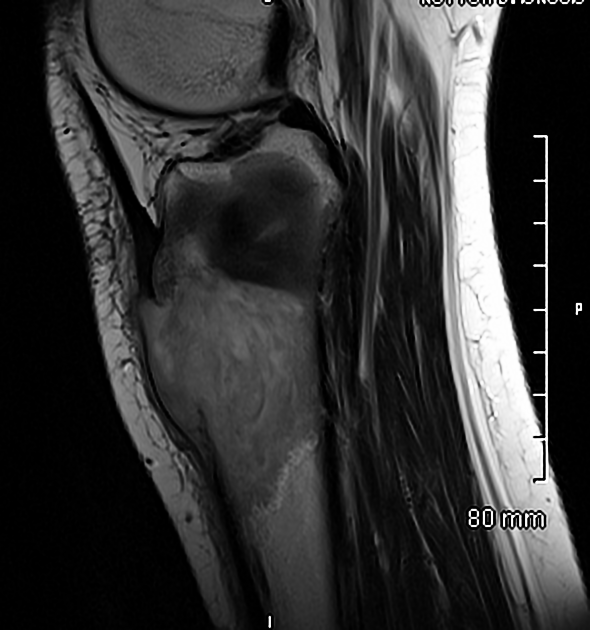
MRI
MRI shows an aggressive bone-forming tumour with bone destruction and often with soft tissue extension and plays an essential role in assessing local tumour extent, including joint involvement and the detection of skip metastases 8-10. Whole-body MRI with DWI can be used for the detection of distant skeletal metastases 9.
Signal characteristics
T1: heterogeneous low to intermediate signal
T2: heterogeneous high signal with low signal areas
STIR/IMFS: high signal with haemorrhagic and hypointense areas
T1 C+ (Gd): enhancement of viable tumour and hypointense non-enhancing ossified parts
It is of note that native T1 weighted images are considered most accurate in predicting medullary involvement or intraosseous tumour extent 8-12, whereas fluid-sensitive sequences are used for evaluation of soft tissue extension 9,10. Septonodular or rim enhancement suggests a chondroblastic subtype 8,9.
Nuclear medicine
FDG-PET shows increased glucose metabolism and is considered sensitive in the detection of distant metastases 9,10.
Radiology report
The radiological report should include a description of the following:
form, location and size
osteoid matrix, growth pattern
tumour margins and transition zone
periosteal reaction, cortical erosion, cortical breakthrough
soft tissue extension and neurovascular involvement
epiphyseal extension
-
joint involvement 8:
intraarticular mass with disruption of synovial membrane or cartilage
joint effusion or its absence
skip metastases
distant metastases
Treatment and prognosis
Management consists of wide surgical resection combined with neoadjuvant and postoperative chemotherapy 1-4 with multiple agents 1,13-15 traditionally including methotrexate, adriamycin, cisplatin and ifosfamide. Nowadays limb-salvage techniques are often used. Radiation therapy plays a role in the setting of unresectable tumours 1.
Prognosis hugely depends on metastatic spread at the time of diagnosis, histological response to neoadjuvant chemotherapy, location of the primary tumour, and surgical resection margins.
Approximately up to 70% of patients with localised disease are long-term survivors. This can increase to >80% in the setting of good response to chemotherapy (defined as ≥90% tumour necrosis) and complete resection with negative margins. On the other hand patients with recurrent or metastatic disease show a low survival rate of <30% and poor response to neoadjuvant therapy as well as incomplete resection are poor prognostic factors as well as proximal extremity or axial skeleton involvement or large tumour size 1.
Differential diagnosis
Lesions that look similar to conventional osteosarcomas on imaging studies include the following entities 4:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.