The CT neck protocol serves as a radiological examination of the head and neck. This protocol is usually performed as a contrast study and might be acquired separately or combined with a CT chest or CT chest-abdomen-pelvis. On rare occasions, it will be performed as a non-contrast study. Depending on the clinical question it might be acquired as double acquisition with a CT angiogram or as a single acquisition e.g with a mono- or biphasic technique.
Note: This article aims to frame a general concept of a CT protocol for the assessment of the head and neck. Protocol specifics will vary depending on CT scanner type, specific hardware and software, radiologist and perhaps referrer preference, patient factors e.g. implants, specific indications.
Contrast doses apply for CT examinations in adults.
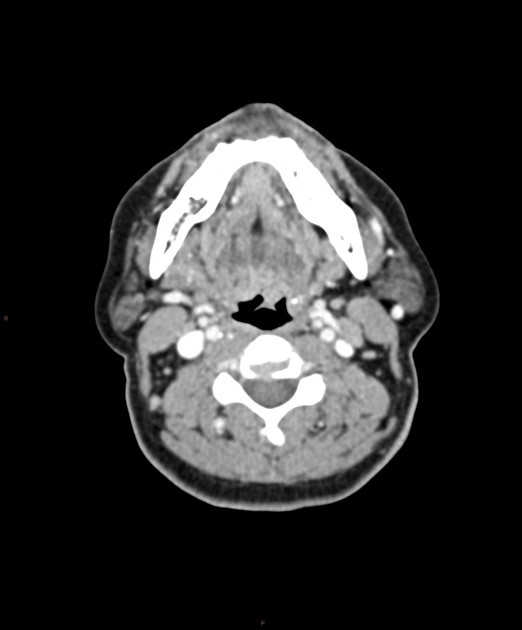
A typical CT of the neck might look like as follows:
On this page:
Images:
Indications
Typical indications include the following 1-5:
inflammatory or infectious processes
head and neck cancer therapy response and follow up
head and neck trauma
bleeding/epistaxis
congenital anomalies
Purpose
In the setting of inflammatory or neoplastic processes, the purpose of a CT neck is the localisation and characterisation of the respective process its extent and its relation to the adjacent tissues as well as the detection of potential complications.
The search for a foreign body requires its localisation. Because contrast material may pose a confounding factor the examination should be performed as a non-contrast study 1.
In the setting of head and neck trauma, the evaluation includes the detection and characterisation of maxillofacial fractures, laryngotracheal injuries, and fractures to the skull base and cervical spine 2,3.
In the setting of thyroid disease, a CT of the neck is usually performed as a non-contrast study and should demonstrate the retrosternal or full extent of the thyroid gland.
Technique
-
patient position
supine position
both arms next to the body, shoulders pulled down
-
tube voltage
≤120 kVp
-
tube current
as suggested by the automated current adjustment mode
-
scout
mid-chest to vertex
-
scan extent
frontal sinus to the aortic arch
depending on the clinical question might exclude the orbit to save radiation on the eye lens
-
scan direction
craniocaudal
-
scan geometry
field of view (FOV): 140-200 mm (should be adjusted to increase in-plane resolution)
slice thickness: ≤0.75 mm, interval: ≤0.5 mm
reconstruction algorithm: soft tissue, bone or other high resolution
contrast injection considerations
non-contrast (e.g. foreign body, thyroid disease)
contrast volume: 70-100 mL
-
biphasic injection technique (inflammatory conditions)
50-60 ml contrast media at 1-2 mL/s
40-50 ml contrast media followed by 30-50 ml saline chaser at 2-3 mL/s starting after 60 seconds
scan delay: 80-100 seconds
-
monophasic injection technique (parotid tumours)
70-100ml followed by 30-50 ml saline chaser at 2-3 mL/s
scan delay: 40-50 seconds
-
respiration phase
-
single breath-hold
inspiration
or puffed cheeks
or valsalva manoeuvre
-
-
multiplanar reconstructions
sagittal images: sagittal aligned through the centre of the vertebral bodies and the chin
coronal images: coronal aligned to the transverse processes and the mandibula
axial images: perpendicular to the head-neck axis
slice thickness: soft tissue ≤3 mm, overlap >30%, bone ≤2 mm
Dynamic manoeuvres for neck imaging
The anatomical complexity of the neck makes radiological assessment difficult; hence the dual phase neck component to delineate structures, there are differing breathing instructions to aid in assessment 9
-
puffed cheeks
creates a negative contrast within the oral vestibule and helps improve the definition of mucosa, buccinator, pterygomandibular raphe, and retromolar trigone
-
valsalva manoeuvre
distends the airway and helps with the visualisation of the paraglottic fat planes
Practical points
patient positioning before scanning might reduce and facilitate multiplanar reconstructions
reconstructions in both standard kernel and high-resolution kernels
in the setting of trauma separate reconstructions of the cervical spine should be obtained from the raw data set
place markers in the setting of palpable lumps and bumps
depending on the exact indication the scan might require an extension of the scan field
-
dose optimisation
use iterative reconstruction algorithms if available
try to minimise acquisitions (e.g with a biphasic injection protocol)
-
imaging in the setting of implants
use monochromatic reconstructions in dual-energy CT scans
use additional wide window setting






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.