Cyanide poisoning is a cause of an acute anoxic-ischaemic encephalopathy that also has eventual chronic sequelae.
On this page:
Epidemiology
Acute cyanide poisoning is rare and often occurs after oral ingestion of cyanide-containing compounds with suicidal intent. However, there are other non-intentional causes such as after smoke inhalation 1,2. Chronic cyanide poisoning is generally related to occupational exposure, such as working in the metal industry 1.
Clinical presentation
Patients can present with a variety of devastatingly disabling clinical features, often manifesting within minutes of exposure 1-5: Patients may present with a bitter almond odour.
headache
seizures
agitation
mydriasis
cardiac arrhythmias
cardiac and respiratory arrest, often leading to coma and rapid death
If a patient survives the acute poisoning, eventual chronic neurological sequelae include the development of movement disorders (e.g. parkinsonism, choreoathetosis, dystonia), or rarely, the development of memory impairment 1-5.
Pathology
A cyanide is a compound, known simply as a 'cyanide', that contains a cyanide group (CN-) 1,3-6. These compounds include solids, typically cyanide salts (e.g. potassium cyanide), liquids or gases (e.g. hydrogen cyanide), which can cause toxicity through ingestion, dermal absorption, or inhalation 1,3-6. It is highly toxic, with the mean lethal dose of potassium cyanide only being 3 mg/kg 1.
Cyanide is a respiratory chain metabolism toxin that inhibits the mitochondrial enzyme cytochrome c oxidase, a terminal enzyme of the respiratory electron transport chain 1,3-6. This culminates in cytotoxic anoxia in cells, especially those that have high oxygen requirements 1,3-6. In the brain, the structures that require the highest oxygen requirement, namely the basal ganglia and cerebral cortex, are the regions most prominently affected by this anoxic toxicity 1,3-6. Thus, the basal ganglia undergoes haemorrhagic necrosis and the cortex undergoes pseudolaminar necrosis 1,3-6. Notably and unusually, despite its rich oxygen supply, the hippocampi are characteristically spared in this process 1,3-6.
Radiographic features
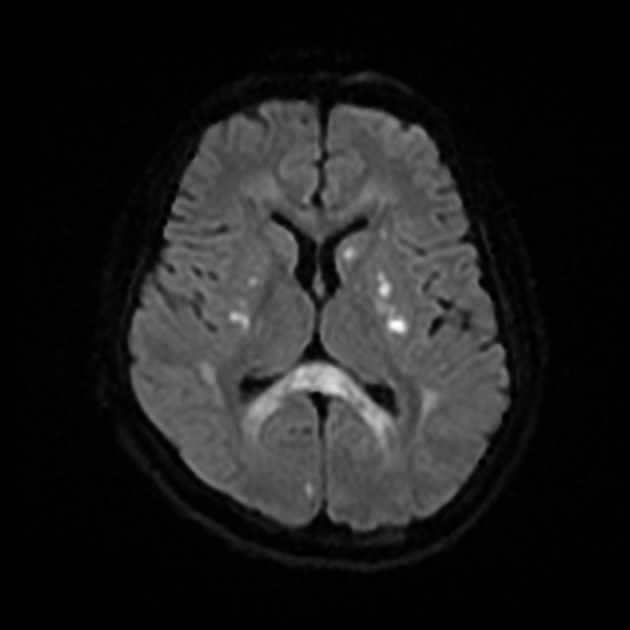
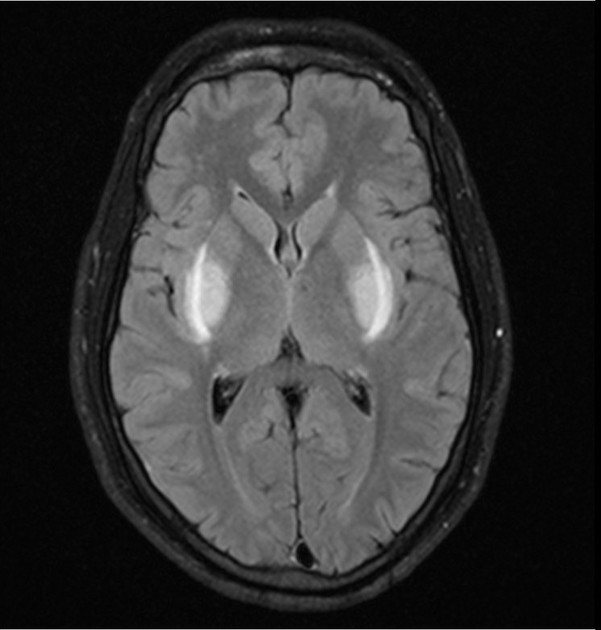
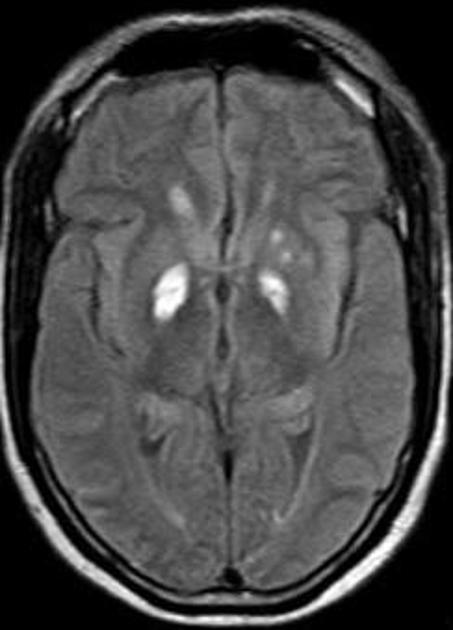
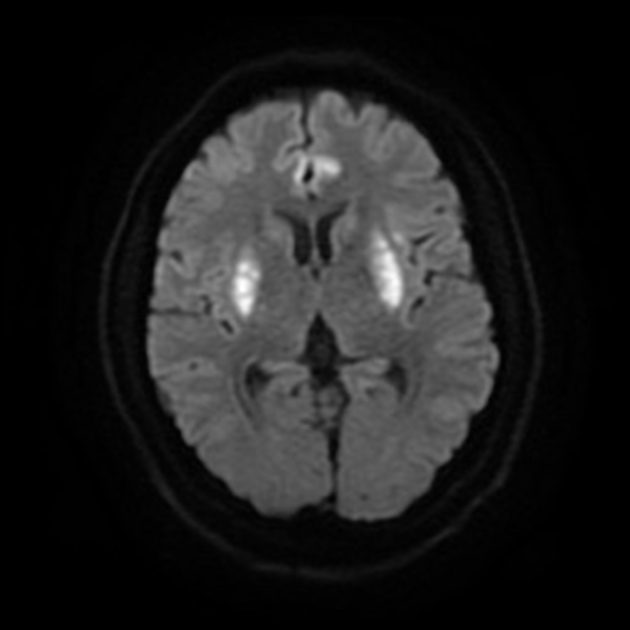
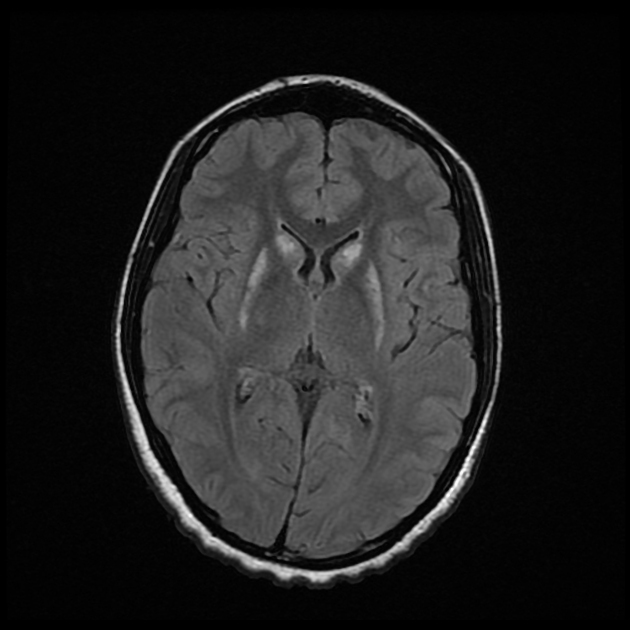
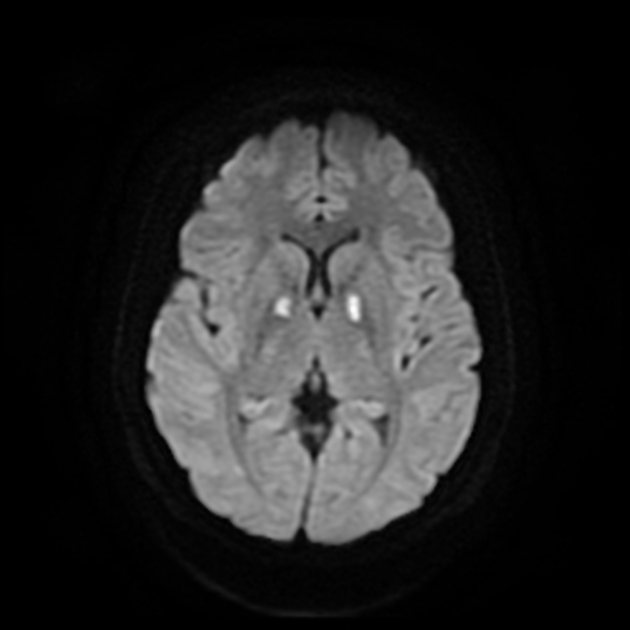
Cyanide poisoning characteristically tends to bilaterally affect the basal ganglia, especially the striatum, and the cerebral cortex, especially the sensorimotor cortex 1,3-6. However, in severe cases that lead to rapid death, more widespread changes, including diffuse cerebral oedema, can be seen 7.
CT
Classically seen as hypoattenuation bilaterally in the basal ganglia, reflective of necrosis. These areas may or may not have evidence of hyperattenuating macroscopic haemorrhage 5. Cortical changes are often not evident on CT 5.
MRI
Regions of involvement are identical to those involved on CT, but are appreciated in greater detail. Signal characteristics of the necrosis in the acute setting include 1,3,4,7:
T1: generally high signal, consistent with pseudolaminar necrosis when affecting the cortex, but also due to presence of haemorrhage
T2/FLAIR: affected areas demonstrate high signal that become more pronounced within weeks
T1 C+ (Gd): usually vivid contrast enhancement
DWI: affected areas show increased diffusion signal
In the chronic phase after acute cyanide poisoning, a decrease of high signal intensity in all sequences is generally appreciated, but this may take more than a year to occur 1,3. Unlike other toxic encephalopathies, such as methanol poisoning, cystic sequelae usually do not eventuate 3.
Treatment and prognosis
Treatment generally involves administration of antidotes such as hydroxycobalamin, which binds to cyanide compounds to create non-toxic compounds that can be safely excreted by the kidneys 2. Another commonly used antidote is sodium thiosulphate, which accelerates the metabolism of cyanide to less toxic derivatives 2.
The prognosis of acute cyanide poisoning is very grim, with a 95% mortality rate 1.
Differential diagnosis
For involvement in and around the basal ganglia, consider:
-
mitochondrial encephalopathies
-
metabolic disorders





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.