Cytotoxic cerebral oedema refers to a type of cerebral oedema, most commonly seen in cerebral ischaemia, in which extracellular water passes into cells, resulting in their swelling.
The term is frequently used in clinical practice to denote the combination of true cytotoxic oedema and ionic cerebral oedema. As the pathophysiology of these two types of oedema is different, as is their imaging, they are discussed separately. The remainder of this article is concerned with true cytotoxic oedema, also known as cellular oedema 8.
On this page:
Images:
Pathology
Cytotoxic oedema is the result of cells being unable to maintain ATP-dependent sodium/potassium (Na+/K+) membrane pumps which are responsible for high extracellular and low intracellular Na+ concentration 6. When energy fails, as is the case in cerebral ischaemia, these pumps cease to operate and Na+ accumulates within the cell, drawing with it chloride (Cl-) and water along an osmotic gradient. This, in turn, results in cellular swelling and a reduction in the extracellular volume 9. These are the primary reasons for increased restricted diffusion on MRI.
This intracellular oedema mainly affects grey matter but also involves white matter as astrocytes are also involved.
In contrast to vasogenic cerebral oedema, in which the blood-brain barrier is compromised, cytotoxic oedema does not involve endothelial dysfunction or changes in capillary permeability.
Radiographic features
CT
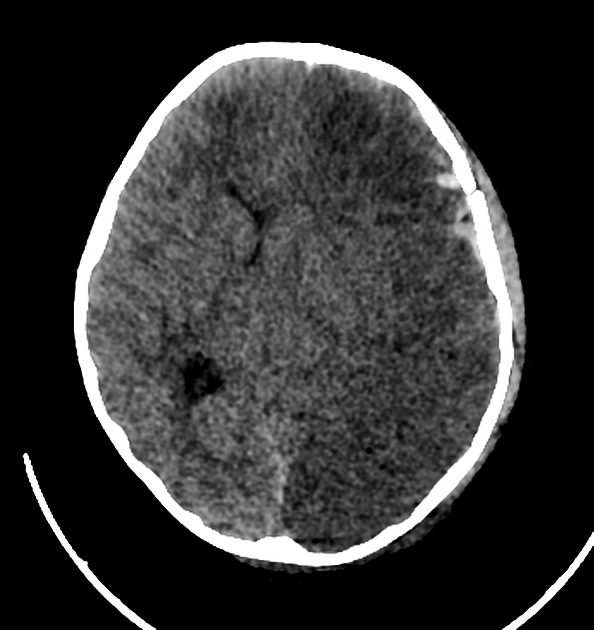
In true isolated cytotoxic oedema little change is evident on CT as a mere redistribution of water from extracellular to intracellular compartments does not result in attenuation changes. The changes colloquially ascribed to 'cytotoxic oedema' are in fact mostly due to ionic oedema and are described separately. This is why brain CT is often normal in patients with an acute ischaemic stroke.
MRI
As cytotoxic oedema represents the redistribution of water from extracellular to intracellular compartments, without a change in local constituents it stands to reason that no T1 or T2 changes are evident. As is the case with CT, the changes colloquially ascribed to 'cytotoxic oedema' are in fact mostly due to ionic oedema and are described separately.
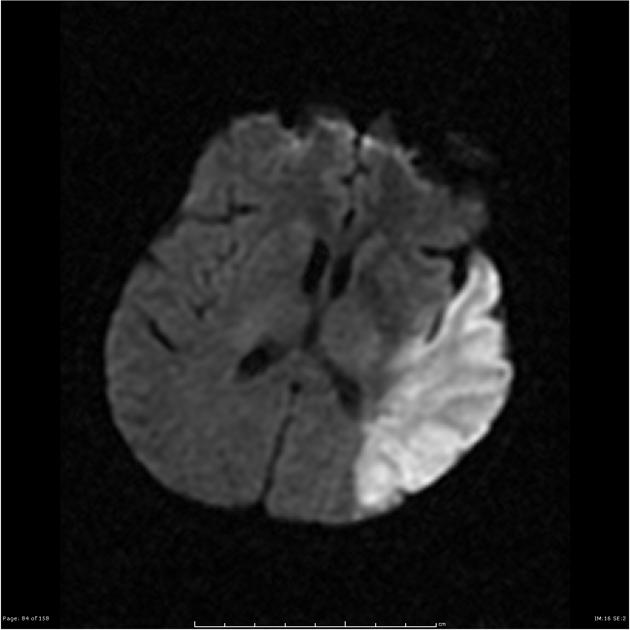
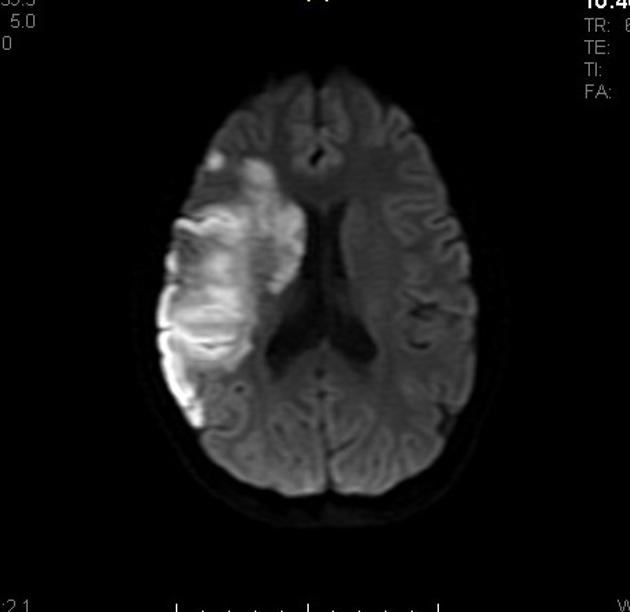
The one sequence which is able to identify cytotoxic oedema, and was thus responsible for a revolution in the imaging of acute ischaemic stroke, is diffusion weighted imaging (DWI). As cells swell due to inward shift of water, there is a commensurate decrease in diffusion, identified as high signal on DWI and low signal on ADC.
These changes persist into the subacute phase until about two weeks when the ADC signal begins to rise above the normal parenchyma and eventually becomes hyperintense.
Treatment and prognosis
Treatment generally focuses on the underlying cause of cerebral oedema. Steroids are not beneficial in the treatment of cytotoxic oedema secondary to stroke, and may, in fact, be harmful in cytotoxic oedema from trauma 7.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.