Dacryocystitis is the inflammation of the nasolacrimal sac related to impairment in the lacrimal drainage system and superimposed infection.
On this page:
Epidemiology
Dacryocystitis has a bimodal distribution: neonates due to congenital abnormalities and when acquired, usually affect individuals older than 40 years of age 3.
Clinical presentation
Dacryocystitis is typically characterised by epiphora, erythema, and oedema in the region of the medial epicanthus and lacrimal puncta as the result of an infection of the nasolacrimal sac. There is often mucopurulent discharge from the puncta and associated conjunctivitis.
Pathology
Obstruction or stricture of the nasolacrimal drainage is an underlying factor.
Most cases in infants represent congenital abnormalities, such as incomplete canalisation or atresia of the nasolacrimal duct, dacryocystocele and facial clefts. Whereas in adults it is usually the result of an acquired abnormality, including:
-
inflammation/infection
rhinitis/sinusitis
nasal septal abscess
-
anatomic variation
enlarged turbinates
-
tumour
iatrogenic/trauma
foreign bodies
The microbiology of dacryocystitis mimics normal conjunctival flora in most instances.
In chronic dacryocystitis, there may be superinfection with fungal species.
Radiographic features
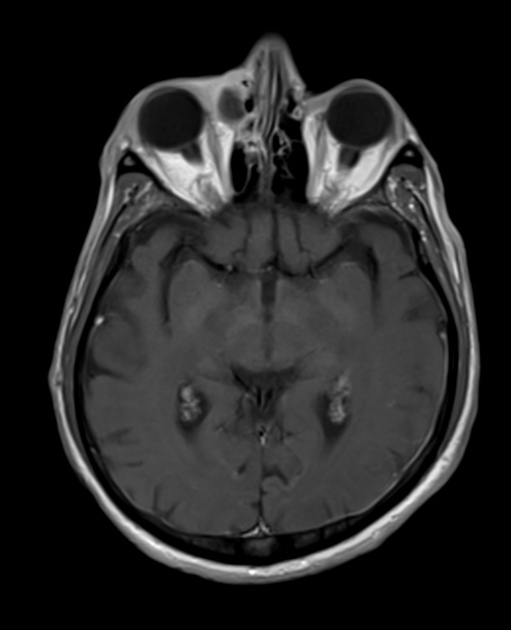
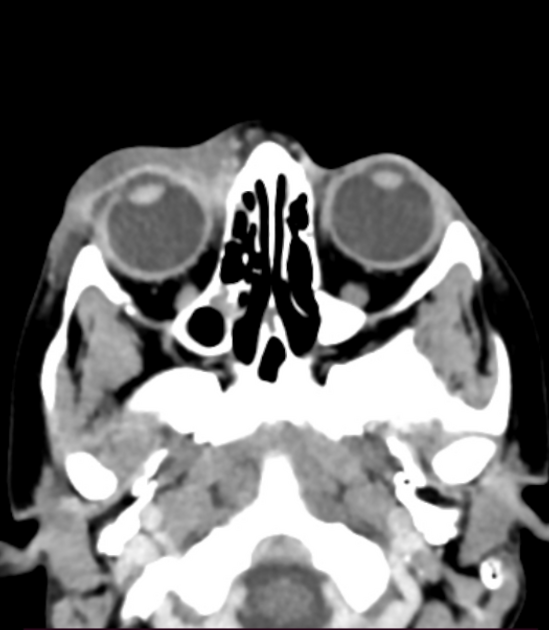
Diagnosis is usually made clinically; however, imaging may help to exclude complications. Imaging is indicated to exclude orbital cellulitis or orbital abscess; both of which are uncommon as the orbital septum acts as a barrier preventing post septal spread 3.
CT findings include well-circumscribed round lesions with peripheral enhancement around the inner canthus, with adjacent soft tissue thickening and fat stranding,
Treatment and prognosis
Treatment is usually with antibiotics in the acute phase. In some cases, intervention (including external dacryocystorhinostomy) may be necessary.
Chronic dacryocystitis typically requires surgery or an interventional procedure.
Complications
abscess formation
fistula formation
sepsis
Differential diagnosis
Differentials on imaging include:
-
anterior ethmoidal cells sinusitis
ethmoidal bone erosion
-
can co-exist with dacryocystitis
-
preseptal orbital cellulitis
can co-exist with dacryocystitis







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.