Diffuse idiopathic skeletal hyperostosis (DISH), also known as Forestier disease, is a common condition characterised by bony proliferation at sites of tendinous and ligamentous insertion. It primarily affects the spine of older individuals. On imaging, it manifests as flowing bridging anterior vertebral osteophytes, most prominent in the thoracic spine, and enthesopathy particularly around the pelvis. The presence of flowing anterior ossification spanning at least four vertebral levels with preserved disc spaces is often used to define the disease.
On this page:
Epidemiology
DISH is more common with increasing age 23, and is most common in the 6th to 7th decades 3. The estimated prevalence is ~15% (range 3-42%) with a male predominance 6,23,24. The prevalence appears higher in developed countries.
Risk factors
chronic isotretinoin use (retinoid medication used for cystic acne) 26
Diagnosis
The Resnick and Niwayama criteria remain the most widely used in the imaging diagnosis of DISH (c. 2021 24), requiring 19:
flowing osteophytes over at least four contiguous vertebrae of the thoracic spine
preservation of intervertebral disc space without extensive degenerative intervertebral disease
absence of facet and costovertebral joint ankylosis
absence of sacroiliac joint (SIJ) erosion, sclerosis or fusion*
However, this represents end-stage DISH and others ref have suggested using a vertebral span of three or even two levels in the setting of prominent extra-spinal enthesopathy. Other criticism includes that only axial manifestations form part of these criteria 24.
*NB SIJ enthesophytes have subsequently been shown to common in patients with DISH 22.
Clinical presentation
DISH is often asymptomatic and identified as an incidental finding on imaging performed for other reasons 23. However, back pain and spinal stiffness are common symptoms in patients with DISH although it is unclear if this is specific to the diagnosis of DISH 23. Similar symptoms of pain and stiffness in the peripheral joints have been reported 23.
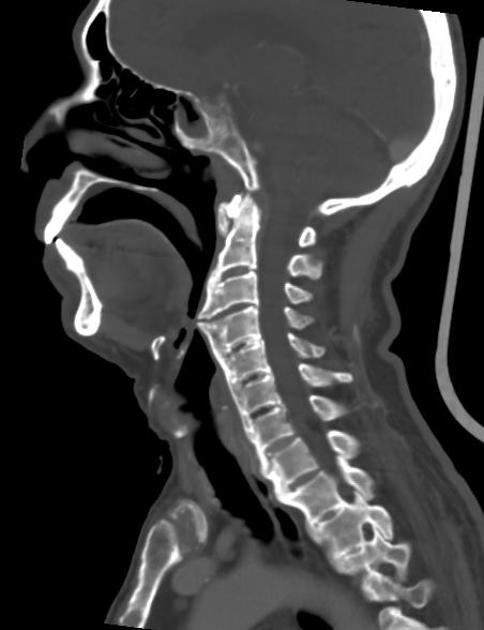
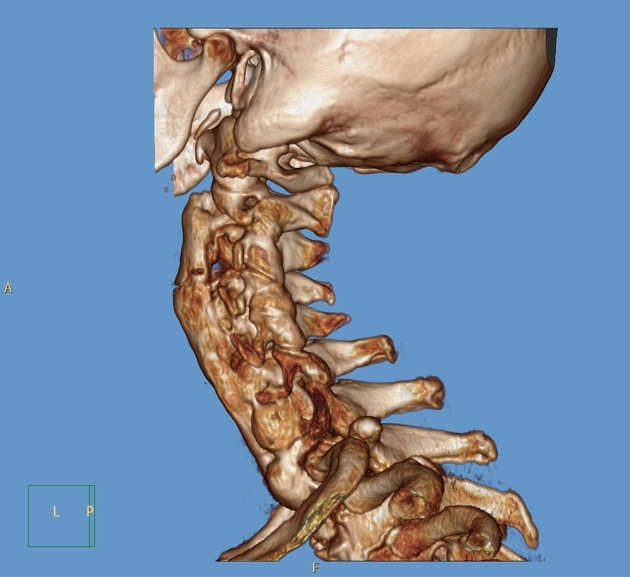
When DISH affects the cervical spine, dysphagia, airway obstruction, and/or difficult tracheal/oesophageal intubation may occur from mechanical compression due to anterior cervical bone production upon the hypopharynx and upper oesophagus 22,23.
Spinal fractures, following even low impact trauma, may be a presenting scenario if DISH results in spinal ankylosis 23.
Pathology
The aetiology of DISH is unknown (c. 2020) 23 but likely involves an imbalance of growth factors and inhibitors leading to excessive bone formation. Histopathological features of spinal DISH include 5:
-
focal or diffuse calcification and/or ossification of the anterior longitudinal ligament
controversial as some studies have shown ALL not to be involved 23
ossification of the paraspinal connective tissue and annulus fibrosus
degeneration of the peripheral annulus fibrosus fibres
anterolateral extensions of fibrous tissue
hypervascularity
chronic inflammatory cellular infiltration
periosteal new bone formation on the anterior surface of the vertebral bodies
The rate at which the ossification progresses is reported to be around one vertebral space bridged every 10 years 14. The bone outgrowth begins at the anterior vertebral body above and below the disc.
Location
-
thoracic spine (most common) 22
right anterolateral ossifications: particularly T7-T11 5
descending aortic pulsation prevents it on the left (opposite occurs if there is situs inversus)
cervical spine: anterior ossification, maximal at lower half of vertebral body
-
upper lumbar segments commonly involved 22
osteophytes are usually bilateral 22
implies advanced/late disease
-
pelvis (common) 22
sacroiliac joints: bridging osteophytes located ventrally
-
pelvic enthesophytes are thought to be highly characteristic 22
gluteus medius origin at the iliac crest and insertion at the greater trochanter
adductor complex origin at the symphysis pubis
hamstring complex origin at the ischial tuberosity
-
appendicular skeleton
enthesophytes around the knee, elbow, ankle 22
involvement of peripheral (e.g. elbow, metacarpophalangeal, glenohumeral) joints not usually affected by osteoarthritis 22
Associations
ossification of the posterior longitudinal ligament: in ~50% of cervical DISH cases 13
metabolic syndrome, hypertension, obesity and diabetes mellitus 23
ossification of the stylohyoid ligament and Eagle syndrome: DISH and ankylosing spondylitis patients both have measurably longer styloid process than controls 16
ankylosing spondylitis: can be both a co-existing condition and differential diagnosis 22
Radiographic features
Plain radiograph and CT
Spinal features
-
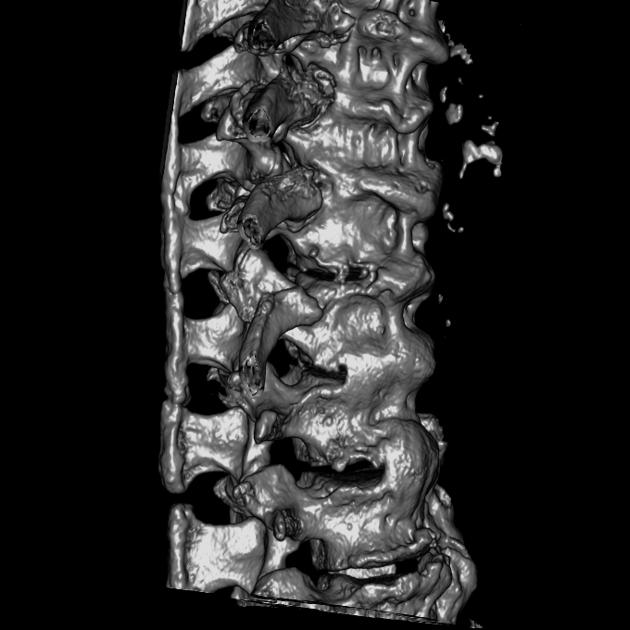
florid, flowing ossification along the anterior or right aspects of at least four contiguous vertebrae 7,22
the left lateral aspect is usually spared in the thoracic spine, thought due to aortic pulsation inhibiting ossification 5
-
osteophytes are largely paraspinal with a linear lucency often seen between the anterior vertebral body cortex and the osteophyte 22
this helps distinguish DISH from degenerative endplate osteophytes and from the syndesmophytes of ankylosing spondylitis 21
disc spaces are usually well preserved: osteophytes/ossification is out of proportion to the degree of disc degeneration 22
-
resultant ankylosis and rigidity is more common in the thoracic than cervical or lumbar spine
frequently incomplete 22
can have interdigitating areas of protruding disc material in the flowing ossifications
no facet joint of costovertebral ankylosis although entheseal bridging may be present 17
chunky ossifications from the lower anterior half of the vertebral body in the cervical spine have been described as being like a candle flame, fall drop, or parrot-beak 22
Sacroiliac features
no sacroiliitis or erosions, however bridging osteophytes anterior to the sacroiliac joints, similar to flowing osteophytes in the spine, are common
posterior bridging osteophytes occur less commonly
the bridging osteophytes may mimic joint ankylosis on x-ray
Extraspinal features
enthesopathy of the iliac crest, ischial tuberosities, and greater trochanters
prominent pelvic enthesophytes are strongly associated with DISH 16
exuberant spur formation in the appendicular skeleton (olecranon, calcaneum, patellar tendon) frequently present
'whiskering' enthesophytes
peripheral joint manifestations including epiphyseal enlargement and joint space narrowing 22
MRI
findings correspond to those on CT
typically true ossification with marrow signal
fat metaplasia at the vertebral corners, and to a lesser degree bone marrow oedema, may occur in DISH, but this is less common than in ankylosing spondylitis 18
Treatment and prognosis
DISH is generally managed symptomatically with analgesics, such as non-steroidal anti-inflammatory drugs, when pain and stiffness are related 23. Managing comorbid conditions like obesity and diabetes mellitus is important.
Complications
Possible complications may require specific treatment:
-
acute spinal fractures, in particular chalk stick fracture, in low impact trauma
inspect the ossified ligaments for disruption, and compare with prior imaging where available to discern fracture from a region without ossification
note that fractures can also occur above or below the rigid segment due to altered biomechanics
dysphagia: resection of osteophytes can relieve mechanical symptoms 23
cervical DISH can make intubation more difficult 11,22
lumbar DISH can cause radiculopathy 11
Differential diagnosis
-
syndesmophytes: thinner, form over the annulus, and are vertically orientated ("bamboo spine")
true sacroiliitis involving the synovial joint (inferior two-thirds) with erosions, adjacent marrow oedema/fat metaplasia and eventual intra-articular ankylosis, as opposed to the para-articular bridging osteophytes seen in DISH
osteoporosis is prominent
may co-exist with DISH 22
-
spinal degeneration (spondylosis)
disc degeneration and height loss
osteophytes arise from the endplates rather than anterior cortex/paraspinal location
anterior longitudinal ligament uncommonly ossified in degenerative disease alone 9
prominent facet and apophyseal joints degenerative changes
-
patients using retinoid acid for skin diseases
skeletal hyperostosis
predominantly involves the cervical spine
-
fluorite intoxication due to long-term ingestion
can cause paraspinal ligament calcification
will have accompanying osteosclerosis, or trabecular blurring/haziness
if seen in a child, consider juvenile idiopathic arthritis (JIA)























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.