Elbow dislocation is the second most common large joint dislocation in adults and the most common in children.
On this page:
Epidemiology
Elbow dislocations are common and account for 10-25% of all elbow injuries in the adult population 1. They are the most common dislocation in children 4.
Associations
If an elbow dislocation is associated with a fracture (fracture-dislocation), it is called "complex." An isolated dislocation without fracture is "simple."
The most common associated fracture in adults is a radial head fracture, although coronoid process fracture is also common. When all of these occur together in a severe posterior dislocation, it is known as the terrible triad of the elbow 1-3. Other elbow fracture-dislocation patterns include the trans-olecranon fracture-dislocation and anteromedial coronoid fractures with associated varus posteromedial instability 6.
The most common associated fracture in children is a medial epicondyle fracture 4.
Clinical presentation
Patients typically present complaining of a painful, swollen joint after a fall on an outstretched hand; also commonly occurs in the context of motor vehicle accidents, violence, and sporting events. In posterior dislocations, the affected elbow is commonly held in mid-flexion, whereas patients with anterior dislocations tend to adopt a position of forearm supination with extension at the elbow. Inspection may reveal a prominent olecranon posteriorly, and the ipsilateral forearm may appear "shortened" compared to the contralateral extremity. The range of motion will be decreased 7.
Complications
Neurovascular structures of note which may be at risk of injury as a complication of elbow dislocations (and potentially during closed reduction attempts) include:
-
most common neuropraxia associated with posterior dislocation
-
median nerve
anterior interosseous branch typically involved
may be entrapped during closed reduction of a posterior dislocation 8
radial nerve
-
brachial artery
associated with anterior dislocations
Pathology
Mechanism
Most elbow dislocations are closed and are most frequently posterior (sometimes posterolateral or posteromedial) although anterior, medial, lateral, and divergent dislocations are also infrequently encountered ref.
The latter (divergent) refers to concomitant ulnohumeral, radiohumeral, and proximal radioulnar joint dislocations resulting in the displacement of the radius and the ulna in opposite directions 10. Posterior dislocation with convergent dislocation (or translocation) of the proximal radiohumeral joint and resultant reversal of their distal humeral articulation has also been described 9.
Posterior dislocations typically occur following a fall onto an extended arm, either with hyperextension or a posterolateral rotatory mechanism 1.
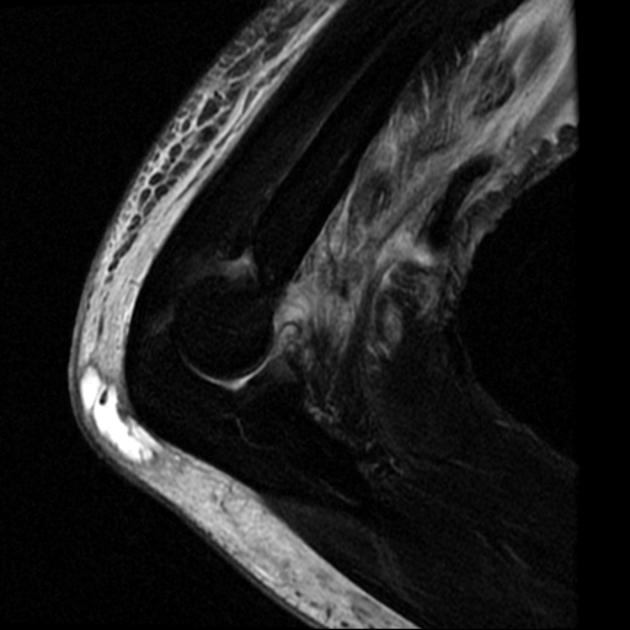
Radiographic features
In most cases, plain films suffice for assessment of elbow dislocations, although CT is increasingly used to pre-operatively assess intra-articular fractures.
Plain radiograph
The dislocation is usually obvious, especially if adequate AP and lateral views are obtained, however, the challenge is in identifying associated fractures.
Although rarely required in practice, a line drawn along the anterior margin of the humerus (anterior humeral line) and one along the long axis of the radius should intersect near the centre of the capitellum 3.
Report checklist
In addition to reporting the presence of a dislocation, a number of features should be sought and commented upon.
-
dislocation direction
posterior, posterolateral, posteromedial, lateral, medial, or divergent
-
associated fractures
most frequently the radial head and coronoid process
other fractures encountered include medial epicondyle (in children), lateral condyle, capitellum, olecranon 2
wrist and shoulder may need to be imaged if there is clinical concern
Treatment and prognosis
When an acute elbow dislocation is simple (i.e. no associated fracture) a non-operative approach is preferred with closed reduction achieved by manual stabilisation of the proximal humerus, pronation of the forearm, longitudinal traction and elbow flexion with manipulation of the olecranon to achieve anatomic reduction 12.
After confirmation of stability through full range of motion and to applied varus and valgus stress a long arm posterior splint with the elbow at 90 degrees of flexion is typically placed; treatment goals in these patients may involve early physical therapy after a short course of immobilisation 1,3.
Failure of closed reduction, or instability thereafter, mandates surgical management; the former is often due to the presence of soft tissue incarceration or the presence of osteochondral fragments 11.
Complex fracture-dislocations of the elbow require operative management, consisting of reduction of the dislocation, management of the fracture, and repair of surrounding damaged soft tissues (ORIF). They are far more likely to have a poor outcome, including secondary osteoarthritis, limited range of motion, instability (~40%), and recurrent dislocation as well as pain 1,5.
Occasionally injury to the brachial artery may be seen (this is more common in open fracture-dislocations) 2.


















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.