Eosinophilic granulomatosis with polyangiitis (EGPA), previously known as Churg-Strauss syndrome is characterized by asthma, eosinophilia and small vessel necrotizing vasculitis and involves the lungs and other organs.
On this page:
Epidemiology
The incidence typically peaks in middle age, 30-50 years of age with pediatric cases being rare 2,16,24. The annual incidence rate of around 0.24-1.78 per 100,000 2,16. There is no gender predilection 24.
Clinical presentation
Clinically, patients with EGPA pass through three phases. Although these do provide a general overview of progression, the phases do overlap 24:
-
allergic prodrome
marked by allergic symptoms typically asthma and sinusitis
may last years
-
eosinophilic phase
eosinophilia
end-organ involvement
-
vasculitic phase
small-vessel vasculitis with end organ damage
Almost all patients have symptomatic asthma and chronic sinusitis. Extrapulmonary signs and symptoms will vary depending on end-organ involvement and the phase of the disease and include diarrhea, skin purpura, arthralgias, renal impariment and neurological symptoms.
Diagnostic criteria
The 1990 American College of Rheumatology criteria requires a positive biopsy for vasculitis and at least four of the six criteria listed below (sensitivity 85% and specificity 99.7%) 16:
asthma: present in almost all patients 2
blood eosinophilia (>10% of the total white blood cell count): present in almost all patients 2,13
mono/polyneuropathy
transient pulmonary infiltrates
paranasal sinus abnormalities: pain or radiographic abnormality
presence of extravascular eosinophils on a biopsy specimen
Pathology
Can be histologically identical to classic polyarteritis nodosa or microscopic polyangiitis. Around 25% of patients will have renal disease, classically necrotizing crescentic glomerulonephritis 12.
Biopsy of parenchymal opacities may show a mixture of necrotizing granulomas, eosinophilic pneumonia, and granulomatous vasculitis 16.
Markers
Anti-neutrophil cytoplasmic antibodies (ANCA) is detected in approximarly half of patients, most often against myeloperoxidase (MPO) (pANCA) 24.
The presence of ANCA has an impact on clinical phenotype, with skin rash, neurological involvement and glomerulonephritis more common in ANCA positive patients, whereas pulmonary, cardiac and gastrointestinal involvement is more common in ANCA negative patients 24.
Radiographic features
Below are the respiratory and cardiac imaging features. Neurological manifestations of EGPA are discussed separately.
Plain radiograph
Chest radiographs are nonspecific but may show:
peripheral consolidation: may be transient/migratory
small pleural effusions: up to 50% of cases 16
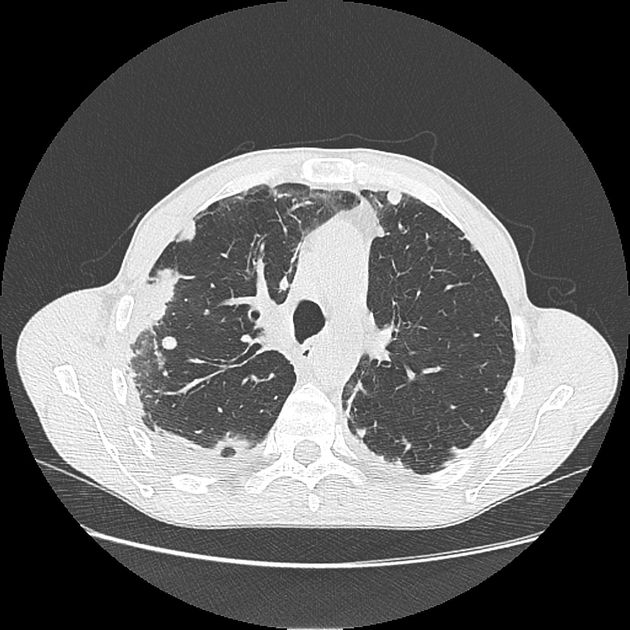
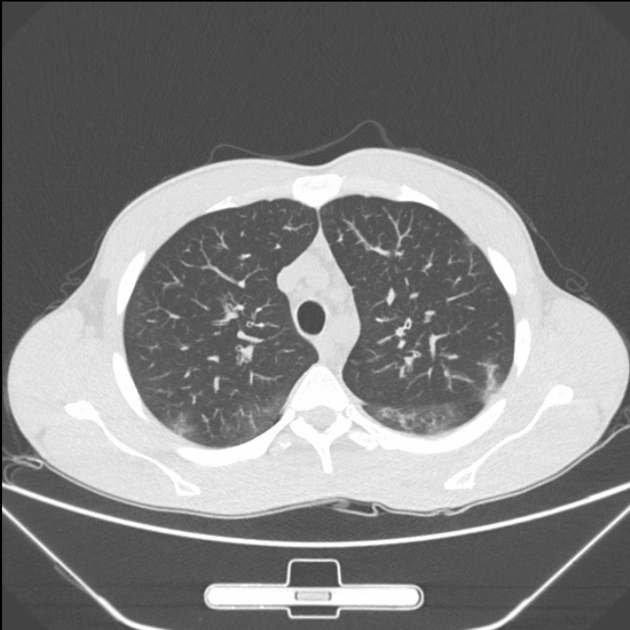
CT
Imaging features include:
-
peripheral or random parenchymal opacification (consolidation or ground glass)
tends to be the most frequent feature 1; can be transient
often bilateral and can sometimes be symmetrical 14
parenchymal opacification is predominantly peripheral or random in distribution 1
-
less common features include
-
features related to eosinophilic infiltration of the bronchial wall and asthma 14
bronchial wall thickening and/or dilatation 5
-
regular and smooth interlobular septal thickening: may reflect the presence of edema secondary to cardiac involvement or eosinophilic septal infiltration 14
cavitation: rare and if present other co-existing pathology should be considered, e.g. granulomatosis with polyangiitis, infection 6
mediastinal lymphadenopathy: seen in less than 25% of cases 16
-
paranasal sinus disease 19-22
nasal polyposis ~75% 22
chronic rhinosinusitis without polyps
MRI
Cardiac involvement clinically manifests in about 66% of patients and can be found in up to 92% of autopsies 16. They include:
-
late gadolinium enhancement: a commonly described finding; can be intramyocardial, subepicardial, or subendocardial 9-10
not confined to one vascular territory (cf. myocardial infarction) 16
myocardial edema: high T2 signal
Treatment and prognosis
Corticosteroids (most commonly prednisone) are the mainstay of treatment. Patients with cardiac, renal, gastrointestinal, or CNS involvement, require additional immunosuppression (e.g. cyclosporine, azathioprine).
The condition generally has a low mortality rate compared with other systemic vasculitides 11. Cardiac involvement may, however, be a significant contributor to disease-related death and may occur in up to 60% of cases 8,13.
History and etymology
Eosinophilic granulomatosis with polyangiitis was first described in 1951 by Jacob Churg (1910-2005), an American pathologist, subspecialising in renal and vascular diseases, and his long-term collaborator and friend Lotte Strauss (1913-1985) an American pediatric pathologist, who were both based at Mount Sinai Hospital in New York City 4,18.
Differential diagnosis
-
granulomatosis with polyangiitis
usually has cavitating nodules
other forms of pulmonary infection






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.